Photoxicity from essential oils is one of the most predictable and incontestable toxic reactions. So much so that even those who tried so hard to tell us that allergic reactions to essential oils were impossible, and were in fact signs of detoxification (they are not!) never contested phototoxicity.
Some plants and essential oils contain molecules that have the unusual talent of binding to the DNA of your skin cells when UV light is also bathing the skin, causing cell death, and this can cause quite a nasty skin reaction, rather like a burn. This is very much a preventable adverse reaction, it simply requires people to be aware of it, and take steps to avoid it.
Phototoxicity is one of two types of photosensitization, the other being photoallergy. Photoallergy is a UV-mediated reaction that involves the immune system and looks more like an allergic reaction (hives) than a phototoxic one (burn). There is also a hyperpigmentation reaction called pigmented contact dermatitis. Very rarely, these two other types of dermatitis are caused by essential oils. Here I will focus on phototoxicity.
Phototoxicity is also known as photoirritation, and the skin reaction is called phototoxic dermatitis, or photodermatitis. When caused by plants or essential oils, it is known as phytophotodermatitis (phyto: plant, photo: light, dermatitis: skin inflammation.) When caused by fragrances it was initially called berloque dermatitis, then bergapten dermatitis, but these terms are rarely used now. Berloque dermatitis comes from the German berlock or the French berloque, meaning trinket or charm. O. Rosenthal coined the term in 1924 to describe pendant-like streaks of pigmentation. This was usually caused by eau de cologne, citrus juice or direct contact with plants.
Why are plants sometimes phototoxic?
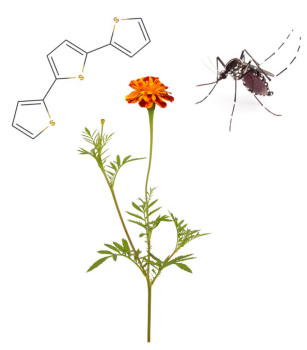
One way that volatile molecules protect a plant is for them to be harmful to a potential herbivore (any creature that eats plants), so that – hopefully – the herbivore learns to avoid plants that smell or taste a certain way. And one of the cunning tricks that plants have evolved to teach herbivores a lesson – whether insects, insect larvae, birds or mammals – is through phototoxicity. For example, methoxsalen, found in limes and rue, is especially toxic to certain butterflies and moths, including the pipevine swallowtail and the tobacco hawk moth, while α-terthienyl, found in taget plants, is toxic to Aedes aegypti, one of the most common types of mosquito. The result is not generally fatal, but may involve damage to various internal organs or, in the case of mammals, phototoxicity to lighter areas of skin such as ears, lips, eyelids and, on cows, udders (Berenbaum 1995).
These compounds rely on sunlight for their toxic effects to manifest. Unlike very tiny creatures, large mammals like cows and humans do not suffer from internal toxicity, as sunlight does not penetrate their dense bodies.
Methoxsalen, mentioned above, is a furanocoumarin (FC), and it is found, alongside others, in parsnips (Pastinaca sativa). This makes the plant toxic to the parsnip webworm – the caterpillar of the parsnip moth (Depressaria radiella) – which otherwise finds parsnips especially delicious. Parsnips are more widely distributed than parsnip moths, and in areas that have no moths, the FCs in the parsnip plants are in lower concentrations than parsnips in areas with moths. When parsnip moths have been newly introduced to a region, parsnips quite quickly ramp up their FCs in response to the threat. The moths then create more detoxifying enzymes, and so the battle continues. This is interesting in its own right, but especially so as it helps explain why the same species of plant, growing in different regions, may vary in the quantity of FCs produced.
The problem
In humans, a phototoxic reaction is rather like getting a surprise sunburn, as the phototoxic chemical exaggerates the skin’s reaction to UV light. The two most relevant sources of UV light are the sun and tanning beds. Common sources of phototoxic chemicals include:
- Fresh lemons and limes
- Phototoxic essential oils
- Phototoxic plants or foods
- Phototoxic drugs
Perhaps because phototoxic reactions are not common, they continue to occur to people who are not aware of the risks. This is in spite of the fact that the phenomenon has been very well understood since 1940.
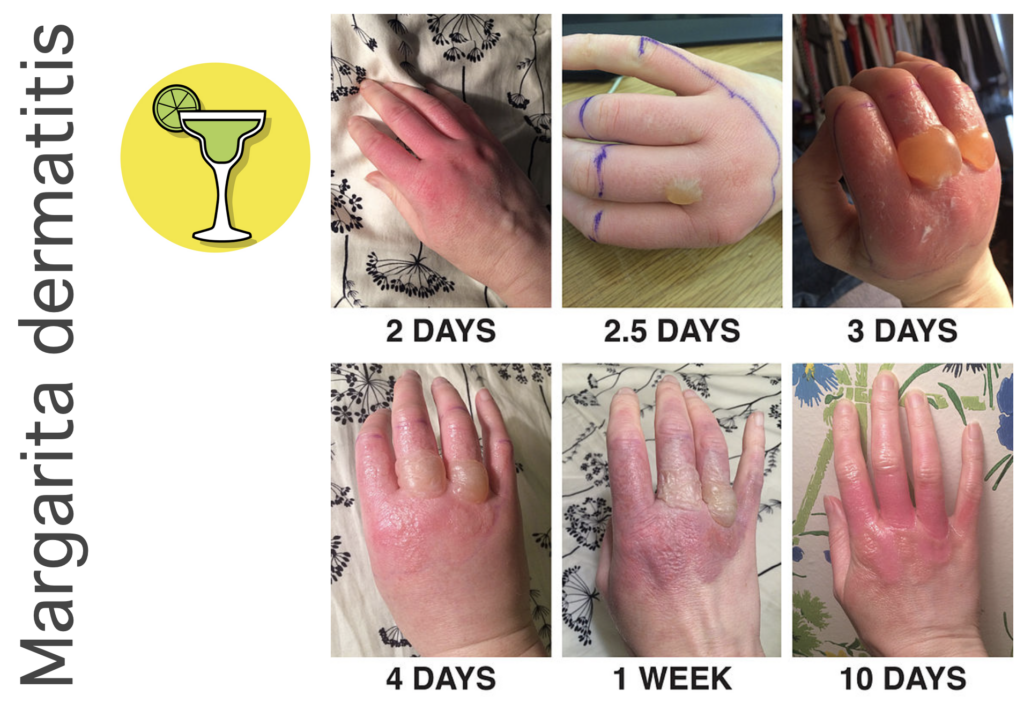
One cause of phototoxic reaction is making margaritas at the beach, because lemon juice and lime juice both contain FCs. And, when you squeeze a citrus fruit, some essential oil usually comes along with the juice. This video shows more the essential oil than the juice, being squeezed out in slow motion. The term ‘margarita dermatitis’ has been used to describe this reaction. The image above is such a case, and it shows the typical progressive worsening over the first 3 days, followed by 7 days of improvement.
Since the late 1970s, the fragrance industry has taken steps to protect consumers by ensuring that fragrant products do not contain levels of phototoxic ingredients that present a risk. However, since the use of essential oils is now so widespread, risk has returned in another form – aromatherapy.
An example of worst-case scenario in regard to essential oils is the case of a lady who applied undiluted Bergamot oil to her limbs in order to help her relax. She then spent 15 minutes in a steam bath followed by 20 minutes under a tanning bed. The steam bath would help the Bergamot oil to penetrate her skin, just in time for the UV radiation from the tanning bed to cause a phototoxic reaction. She was in hospital for a week with extensive burns, and in the image above you can see where a very large blister has burst. Full report HERE.
In 2016 I was asked to be an expert witness in a case where a product containing approximately 20% of Bergamot oil caused a severe phototoxic reaction. The (very large) essential oil seller seemed to have no idea that this could be dangerous.
What it looks like
The visible result often looks like a burn with pigmented skin at the edges. Mild cases either have no pigmentation and just slight burning, or just pigmentation with no apparent burning (see images). There are blisters in more severe cases, and these can be quite large. In the worst cases, burns are full-thickness (3rd degree). If over a large area of skin, patients have been hospitalized for one or two weeks, and there is a risk of anemia due to blood loss, though such severe cases are rare. After the burn heals, patchy pigmentation often remains for weeks or months, but it eventually disappears. It’s thought that the long-term pigmentation may be because melanocytes migrate to the “wrong” layer of skin.
The timing
Phototoxic reactions are insidious in the sense that there is usually no pain or inflammation initially – you don’t know it’s happening when it’s happening. The burns develop hours later, and continue to worsen for 1-3 days. When a phototoxic substance is applied to the skin in sufficient concentration, exposure to UVA radiation any time within the next 12 hours, possibly longer, can cause a phototoxic reaction (Zaynoun et al 1977).
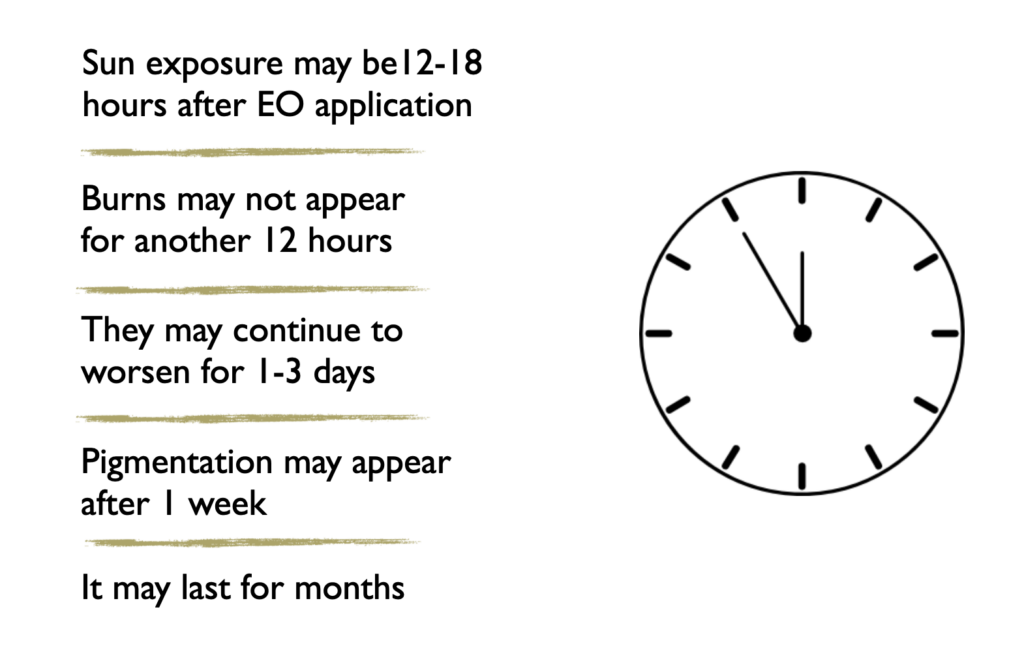 In one case a 15 year-old boy applied undiluted Bergamot oil to his neck to help him sleep one night. Twelve hours later he went outside for an hour or so to play soccer in weather that was partly cloudy. The next morning – 18 hours after the soccer game and 30 hours after applying the essential oil – he woke up to find his neck covered in painful blisters. See images below, and full report HERE.
In one case a 15 year-old boy applied undiluted Bergamot oil to his neck to help him sleep one night. Twelve hours later he went outside for an hour or so to play soccer in weather that was partly cloudy. The next morning – 18 hours after the soccer game and 30 hours after applying the essential oil – he woke up to find his neck covered in painful blisters. See images below, and full report HERE.
Phototoxic chemicals
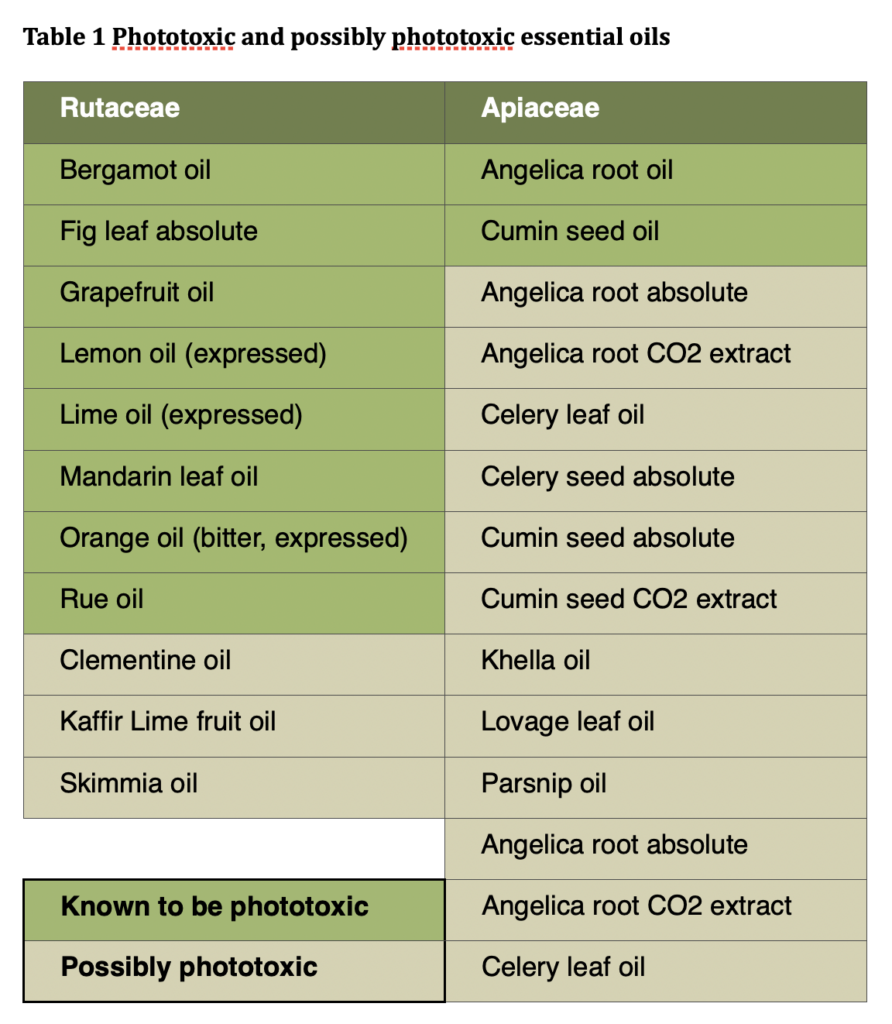
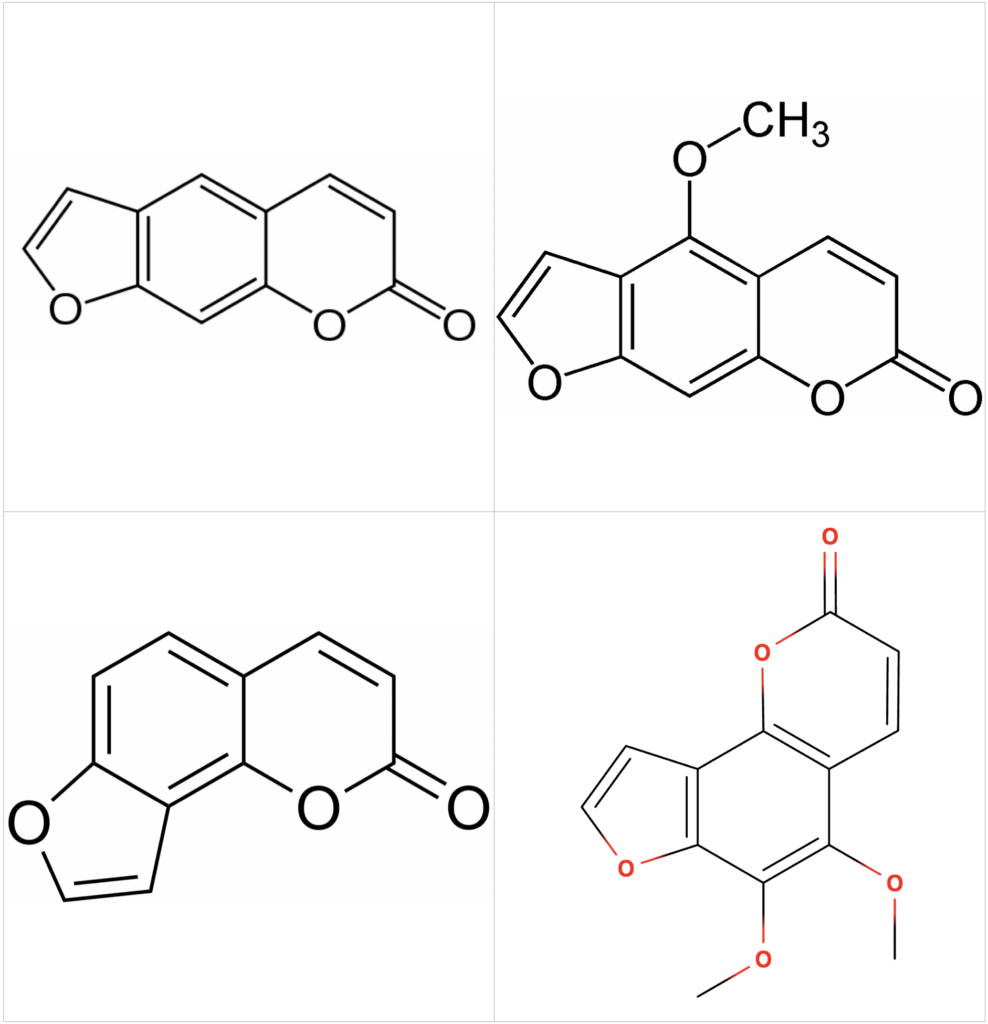
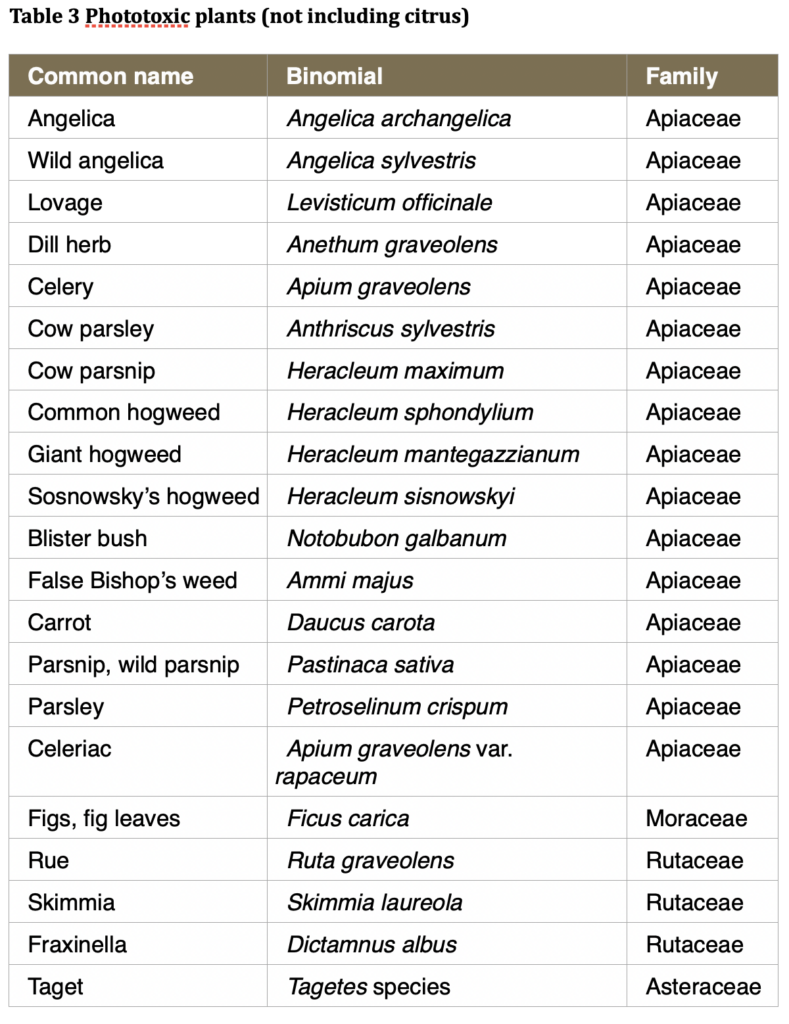
Almost all phototoxic chemicals found in plants belong to a class known as furanocoumarins, also known as furocoumarins. There are quite a few FCs, and their photoxicity varies from negligible to potent. FCs are only present in very small percentages in essential oils, usually less than 1%, but even 0.1% can be phototoxic. FCs are primarily found in two plant families: Apiacea and Rutaceae, though a few Asteraceae, Moraceae and Fabaceae species also contain them. This is shown in Table 1, which includes a “possibly phototoxic” category. These are extracts and oils from plants that do contain FCs, but the essential oils and extracts have not been tested for phototoxicity, and they might or might not contain FCs.
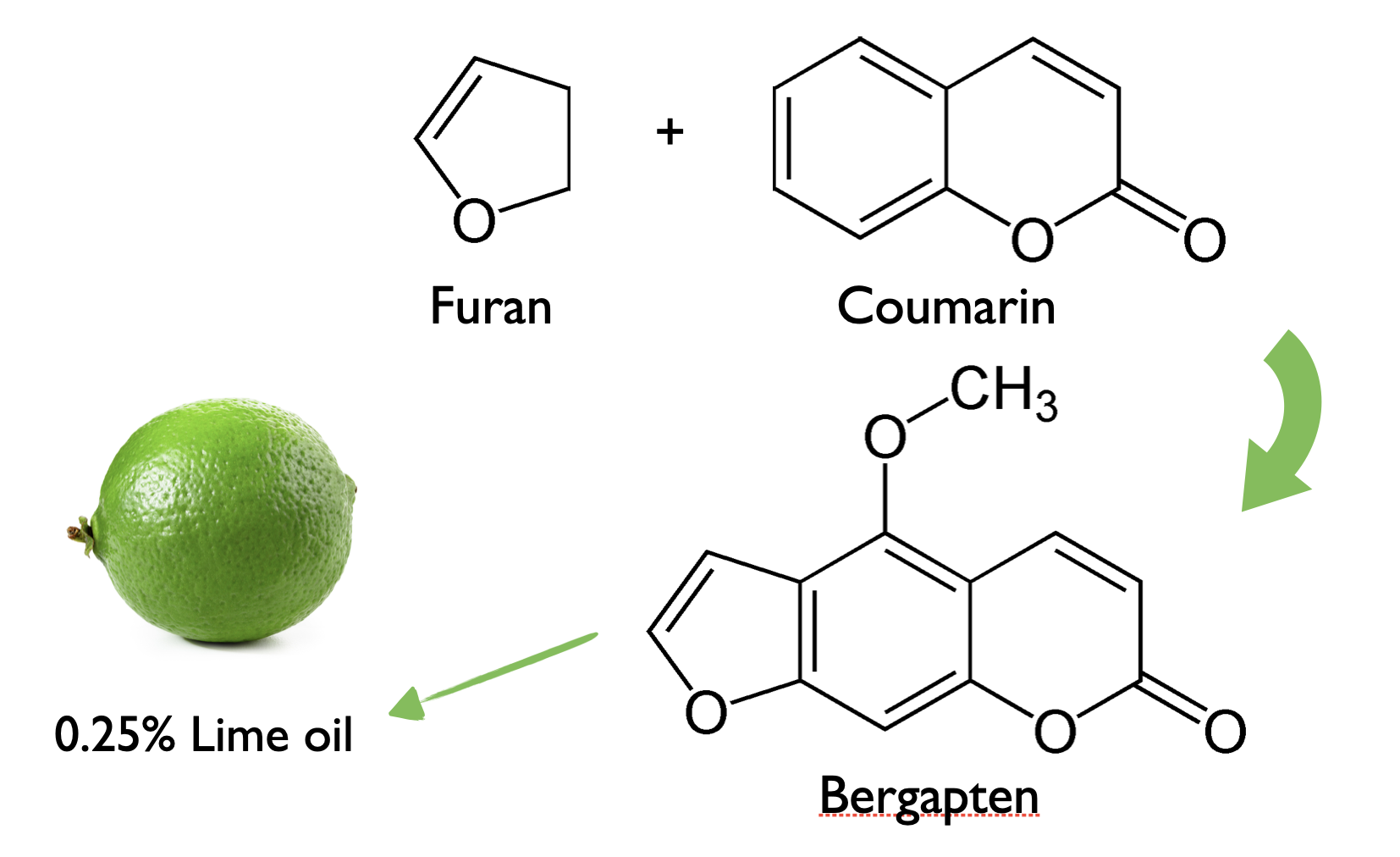
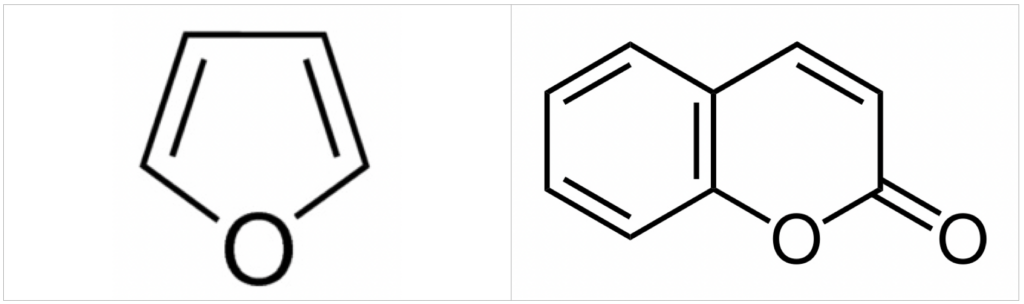
There are two sub-categories of FCs – psoralens and angelicins – each named after a representative molecule. FCs consist of two elements: a coumarin molecule with a furan ring attached. (Coumarin itself is not phototoxic.) Depending on the site of attachment, the FC is either linear, like psoralen, or angular, like angelicin. Bergapten, one of the most prevalent and potent FCs, is a linear molecule, so it’s a psoralen. It is thought that linear FCs are more potent, since they form stronger links with DNA than angular FCs.
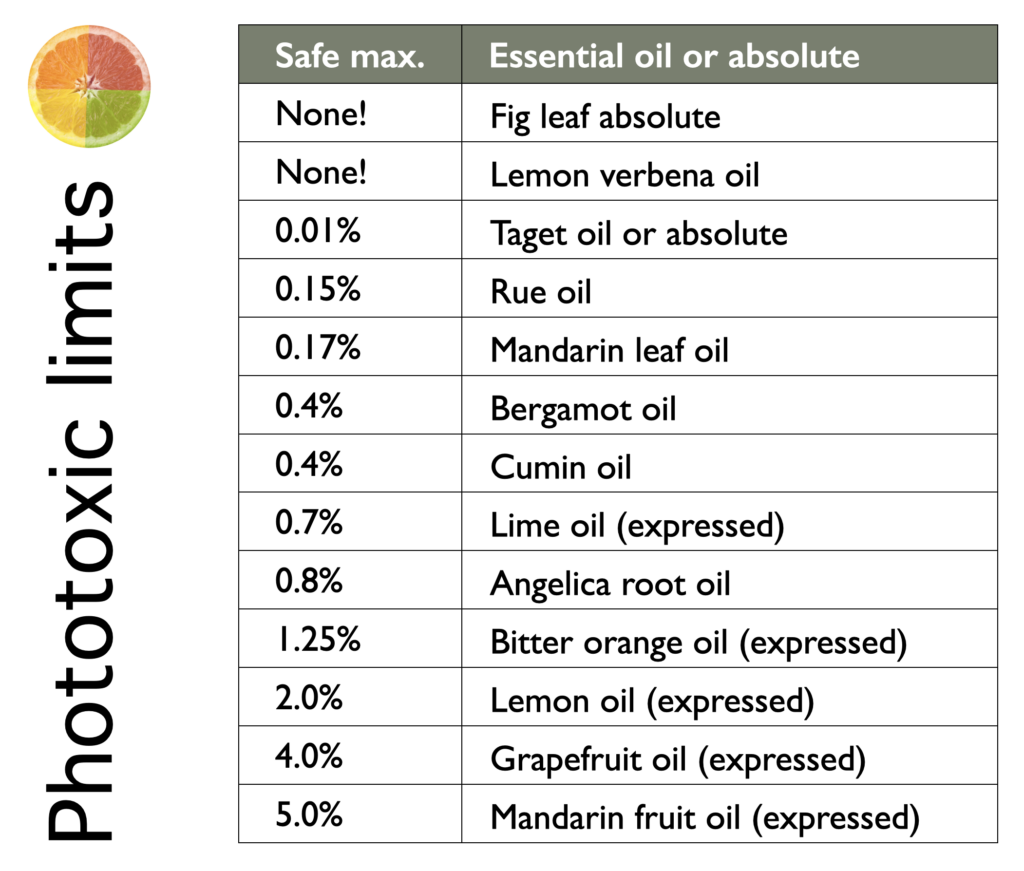
The phototoxicity associated with FCs is avoidable if appropriately low dilutions of the essential oils are used (see Table 2). There are two provisos here. One, if you use more than one phototoxic oil at the same time, and you are at the max level for both, you could have a phototoxic reaction, so you need to use less of both. Two, if you are sunbathing or going under a sunbed, it would be advisable to completely avoid phototoxic essential oils, as even very low levels could possibly present a risk. Another way to avoid phototoxicity is to use an oil that has had the FCs removed, typically by fractional distillation. The most common example of this is bergapten-free Bergamot oil, or Bergamot FCF (furanocoumarin-free).
It’s worth noting that FCs do have therapeutic properties. They do not all demonstrate the same effects, but ones they tend to have in common include anti-inflammatory, antitumoral, hypoglycemic (diabetes) and prevention of osteoporosis (Ahmed et al 2020, Bruni et al 2019, Hung et al 2017, Quetglas-Llabrés et al 2022). Bergapten may also be useful in Alzheimer’s disease and depression (Liang et al 2021). We do not yet know what doses of essential oils would be needed to attain any of these effects, or whether clinical effects are even a realistic expectation. However, depending on the effect we are looking for, using the whole essential oil, with its FCs, often makes sense.
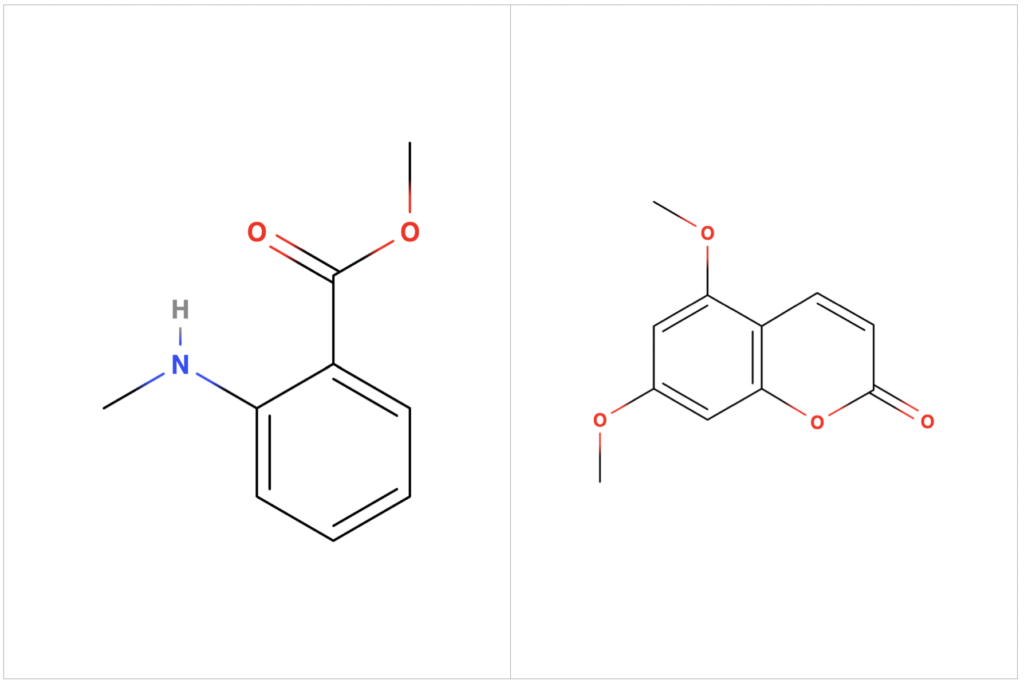
There are a few non-FC phototoxic constituents of essential oils: α-terthienyl, found in Taget species, and dimethyl anthranilate, found in Mandarin leaf. Citropten, also known as limettin is actually a coumarin, not a furanocoumarin, as it does not contain a furan ring (see images at left).
How it works
Whether from ingestion or topical application, when a phototoxic chemical reaches skin cells (keratinocytes) it gets inside the cell and travels to the nucleus. In the presence of UVA radiation, it forms a chemical bond, with the cell’s DNA. These bonds attach to either one (DNA adduct) or two opposing DNA strands (crosslink). Crosslinks are particularly strong, and the DNA helix becomes warped.
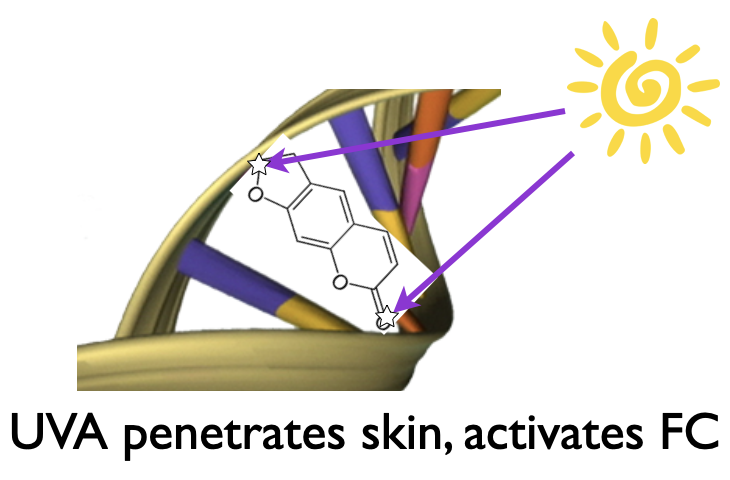 This all happens because the UV light changes the electron spin of the phototoxic molecules to an excited, “triplet” state, which makes them more likely to form bonds. Think of this as electrons becoming even more hyperactive than normal. Ultimately, these adducts and crosslinks cause the death of the skin cells. At the same time there is inflammation, and in many cases melanocytes – the cells that produce the skin pigment melanin – rapidly increase, causing pigmentation.
This all happens because the UV light changes the electron spin of the phototoxic molecules to an excited, “triplet” state, which makes them more likely to form bonds. Think of this as electrons becoming even more hyperactive than normal. Ultimately, these adducts and crosslinks cause the death of the skin cells. At the same time there is inflammation, and in many cases melanocytes – the cells that produce the skin pigment melanin – rapidly increase, causing pigmentation.
If there’s no UV light reaching the skin, the molecule stays in its “unexcited” state, the phototoxic molecule exits the cell, and phototoxicity does not occur (De Almeida et al 2008).
Phototoxicity from essential oils
Phototoxic reactions from fragrances containing certain citrus oils were first reported in 1916, though they were not well understood at that time (see timeline). Since the publication and implementation of IFRA (International Fragrance Association) safety guidelines in the 1970s, phototoxic reactions from commercial fragrances have become very rare.
Citrus fruit oils can be either distilled or expressed. FCs are relatively heavy, non-volatile molecules, meaning that they do not easily evaporate, and so they will not pass over into the essential oil during distillation. Because distilled citrus oils contain virtually no FCs, they are not phototoxic. Expression is a mechanical process that rasps the peel of whole fruits, allowing the essential oil to be collected. They are then extracted for juice. These videos show expression of Lemon oil and Bergamot oil.
Timeline of developments on phototoxicity
1897
Publications from J.J. Stowers in the UK and J.C. White in the USA report on pigmented dermatitis from parsnips and/or angelica. However, neither understood the important role of sunlight.
1916
From E. Freund in Germany, the first report of phototoxic reactions to eau de cologne and to bergamot oil. However, still no understanding of the role of sunlight.
1934-1936
Several researchers demonstrated that the reaction needs sun exposure to follow exposure to a phototoxic plant.
1938
In Germany, H. Kuske demonstrated that furanocoumarins were active ingredients in phototoxic plants. He isolated, and then tested, both bergapten and oxypeucedanin.
1939
In Denmark, Jensen and Hansen demonstrated that certain wavelengths of UV radiation (i.e. UVB) were required to produce a phototoxic reaction.
1942
In England, “phytophotodermatitis” was coined by Robert Klaber, who finally put all the evidence together in a way that made sense.
1967
In Italy, Musajo and colleagues discovered that FCs can enter a skin cell and, under the influence of UVA radiation, can bind to the cell’s nucleus causing cell death.
1974
IFRA publishes safety guidelines for citrus fruit oils. The maximum for Bergamot oil to avoid phototoxicity is 0.4% in leave-on products.
1977
In Scotland, S.T. Zaynoun demonstrated that different vehicles gave different results, as did the skin site, existing pigmentation, and the time lapse between FC application and UV irradiation.
1995
Essential Oil Safety 1e refers to the IFRA safety guidelines for phototoxicity.
1996
IFRA publishes guidelines for furanocoumarins in citrus oils (0.0015% maximum in finished products).
2014
Essential Oil Safety 2e refers to the updated IFRA safety guidelines for phototoxicity
Most of the phototoxic essential oils are expressed citrus oils, but one curiosity about FCs is that they sometimes pass over during distillation into the essential oil (Angelica root, Cumin seed) and sometimes not (distilled Lime or Lemon). It’s not clear why this is, though it would be more correct to say that distilled citrus fruit oils contain very much less FCs, rather than none at all. For example, HPLC analysis showed that a distilled Lemon oil contained 12 times less isopimpinellin, 22 times less bergapten, and 930 times less citropten than an expressed Lemon oil, which means that the distilled oil is not phototoxic, even though it contains some FCs (Li et al 2021). If you’re not sure what the difference is between expression and distillation, go here.
Some essential oils contain extremely small amounts of FCs, not enough to make them phototoxic. These include Caraway, Ginger, Mandarin fruit (expressed), Parsley herb, Patchouli, Tangerine (expressed) and Yuzu (expressed), as well as most distilled citrus fruit oils. For example, Bergamot oil contains about 0.2% of bergapten, and this compares with Tangerine (0.005%), Parsley leaf (0.002%) distilled Lime (0.0003%) and Yuzu (0.0001%).
Bergamot oil normally contains 0.11-0.33% bergapten (Tisserand & Young 2014 p211). It can be re-processed using fractional distillation, in order to remove all, or virtually all of the bergapten. This is known as bergapten-free Bergamot oil, or Bergamot FCF (furanocoumarin-free). Lime, Lemon and Grapefruit oils can also be produced with low or zero FCs. These bergapten-free oils are considered to be non-phototoxic.
Phototoxicity from essential oil ingestion
Since ingested FCs do distribute to the skin, this is theoretically possible, and we know that ingested phototoxic herbs or drugs present a potential risk. However, we also know from something called PUVA therapy that a phototoxic ingested dose of Bergamot oil would need to be in the region of 15 mls. In PUVA therapy, doses of 0.5-0.7 mg/kg body weight of bergapten are given orally in combination with intense UVA exposure, in order to treat certain chronic skin conditions. Since 15 mls is many times higher than any dose used in aromatherapy, the risk from ingested essential oils is likely to be negligible.
Phototoxicity from handling food items or wild-growing plants
A few common food items contain FCs. These include most citrus fruits, parsley herb, dill, parsnip roots, and celery stalks, leaves and roots. Phototoxic reactions have been reported from handling all of these items, and typically involve either picking, peeling or cutting (Ljunggren 1990, Pederson & Arles 1997, Seligman et al 1987). It is theoretically possible to experience a phototoxic reaction from just the ingestion of a food item, though reported cases are rare. There are two case reports of phototoxicity from celery root consumption followed by a tanning bed session (Ljunggren 1990, Puig & Moragas 1994).
Table 3 lists plants that you may encounter, either in your kitchen or outside, and that contain phototoxic chemicals. There are several cases of phototoxic reactions from these plants (Can et al 2011, Cordoba et al 2017, Lagey et al 1995, Moreira et al 2010.). Some of the most severe reactions have been from fig leaves (Abali et al 2012, Bollero et al 2001, Sforza et al 2013, Son et al 2017). A fig leaf infusion or decoction is sometimes applied to the skin as a herbal remedy, and subsequent sun exposure is almost always phototoxic. This is probably because fig leaves contain both psoralen and bergapten, two of the most potent FCs. Fraxinella is also known as burning bush, or gas plant. This is because the volatile oils given off by the plant are prolific, and can allegedly catch fire if lit with a match. This has given rise to the theory that this was the “burning bush” of the Bible.
Phototoxicity from sunscreens
Paradoxically, some sunscreens have been implicated as causing photosensitization, including:
- Benzophenones
- Cinnamates
- Salicylates
- PABA
- Octocrylene
The safest and most effective sunscreens are those based on physical sunscreens, not chemical ones. The physical sunscreens are zinc oxide and titanium dioxide.
Phototoxicity from drugs
There is a long list of potentially phototoxic or photoallergenic medications, and new ones are added on a regular basis. Unlike phototoxicity from essential oils, reactions are unpredictable and inconsistent between individuals. The following list includes some of the most likely oral medications to cause photosensitization. One example is given for each class of drug:
- Tetracylines (Doxycycline)
- Fluoroquinolones (Sparfloxacin)
- Thiazide diuretics (Hydrochlorothiazide)
- Antiarrhythmics (Amiodarone)
- Antipsychotics (Chlorpromazine)
Go here for a much fuller list. It is not known whether the combination of a photosensitizing drug and a photosensitizing essential oil would increase risk. No case has so far been reported.
Risk factors
The severity of the reaction depends on these five factors
1) The amount and potency of phototoxic chemical(s) consumed or applied.
2) The type of topical application (leave-on or wash-off)
3) The time elapsed since application or consumption
4) The intensity & duration of UV radiation
5) The person’s skin phototype
The substance applied
There are safe levels for phototoxic essential oils.
The type of topical application
The risk of phototoxicity from a wash-off product such as soap or bubble bath is considered to be negligible, but phototoxicity can apply to any type of leave-on product such as an oil, gel or lotion.
Skin phototoype
There are six skin phototypes, ranging from “very white” to “very black”. Darker skins are more protected from phototoxicity, but they can still burn, and skin phototype is not taken into account in the safety regulation of citrus oils.
Avoiding phototoxicity
- Don’t use any phototoxic essential oils
- If you intend to sunbathe or go under a tanning bed, avoid phototoxic oils completely.
- If you use phototoxic oils, make sure the concentrations are in the safe zone
- There is negligible risk if the essential oils are in a wash-off product
- If you do use a phototoxic amount, make sure that area of skin is not exposed to UV radiation for at least 12 hours, either by completely covering it, or by not going outside. If you can’t avoid this, sunscreen will help some.
Phototoxicity regulation
Cosmetic safety guidelines are published by The International Fragrance Association (IFRA). IFRA membership consists of most large cosmetics companies, and IFRA members are bound to following the IFRA safety guidelines. For non-members, the IFRA code represents industry best-practice guidelines.
The IFRA guideline for Bergamot oil, to avoid phototoxicity, was introduced in 1974. It states that, for application to areas of skin exposed to sunshine, Bergamot oil should be limited to a maximum of 0.4% in the final product, except for bath preparations, soaps and other wash-off products (IFRA 2009). The IFRA guideline for citrus oils containing furanocoumarins states that, due to the phototoxicity of bergapten, citrus oils should not be used in “leave-on” products such that the concentration of bergapten is greater than 15 ppm.
Similarly, in Europe, essential oils containing FCs must be used so that the total level of bergapten will not exceed: (a) 15 parts per million (ppm) in finished cosmetic products intended for application to skin areas likely to be exposed to sunshine, excluding rinse-off products; or (b) 1 ppm in sun protection and in bronzing products (SCCNFP 2003). The EU regulations are a legal requirement in Europe, but do not apply in the US. However, their existence highlights the general industry awareness of phototoxicity as a material risk to consumers.
Note that, in Europe a “bronzing product”, i.e. one that would be used for tanning in the sun or when using a tanning bed, should not contain more than 1 ppm of bergapten.
To summarize – in order to avoid phototoxicity, the IFRA guideline for Bergamot oil is a maximum of 0.4% in topical “leave-on” products. The IFRA and the EU maximum for bergapten is 15 ppm (0.0015%). For a Bergamot oil with 0.33% of bergapten, this represents a maximum for the essential oil of 0.45%.
IFRA safety guidelines for potentially phototoxic essential oils have been clearly laid out in Essential Oil Safety since 1995 (Tisserand & Balacs 1995, Tisserand & Young 2014). This book represents unofficial safety guidelines for the aromatherapy industry.
Musings and conclusions
I was fascinated to read Dr. Robert Klaber’s 1942 paper, as it includes a detailed account of the scientific theories and explorations of the previous 45 years. Because most early cases happened on beaches, at one point the sea was considered a possible factor. Even when many plants had been identified as causing these odd skin reactions, it was some years before it was realized that sunlight was also a vital factor.
One researcher, in 1931, almost got it right, but in his experiments he irradiated the skin before rubbing it with a phototoxic plant and, unsurprisingly, the results were negative. Another researcher at first thought the cause was a parasite, and later
Finally, in 1936, Hirschberger and Fuchs In Germany were able to reproduce all the characteristic features of phototoxicity by rubbing the skin with wild parsnips, followed by exposure to sunlight. In France, Kitchevatz was able toi do the same thing with various fig extracts. This was followed two years later by Kuske isolating two FCs – bergapten and oxypeucedanin – and demonstrating that they were active molecules in phototoxicity.
Phototoxicity from plants was first observed in ancient times, and by different civilizations, and this knowledge was used to treat vitiligo. It was not until the 1960s that modern phototherapy, combined with ingested FCs for vitiligo was developed in the form of PUVA (psoralen + UVA) therapy. Below are some example reports of phototoxic reactions.
Citrus essential oil cases
Academic reports
Bergamot oil
https://www.ncbi.nlm.nih.gov/pubmed/11511848
https://www.ncbi.nlm.nih.gov/pubmed/9667455
https://www.ncbi.nlm.nih.gov/pubmed/8982544
https://www.ncbi.nlm.nih.gov/pubmed/9601600
Adverse reaction reports
Bergamot oil
Lime oil
Citrus juice cases
Academic reports
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4500699/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1312240/
https://www.ncbi.nlm.nih.gov/pubmed/18395351
https://www.ncbi.nlm.nih.gov/pubmed/11887098
http://www.njmonline.nl/getpdf.php?id=1446
http://www.nejm.org/doi/full/10.1056/NEJMicm053778#t=article
Online posts
https://en.wikipedia.org/wiki/Phytophotodermatitis
http://www.today.com/health/limeburn-citrus-sun-leads-nasty-rash-t38686
http://www.polkmoms.com/forum/topics/children-severly-burned-by-household-fruit
References
Abali, A. E. S., Aka, M., Aydogan, C., & Haberal, M. (2012). Burns or phytophotodermatitis, abuse or neglect. Journal of Burn Care & Research, 33(6), e309–e312. http://doi.org/10.1097/BCR.0b013e318257d8771111
Ahmed, S., Khan, H., Aschner, M. et al (2020). Anticancer potential of furanocoumarins: Mechanistic and therapeutic aspects. International Journal of Molecular Sciences, 21(16), 1–20. https://doi.org/10.3390/ijms21165622
Berenbaum, M. (1995). Phototoxicity of plant secondary metabolites: insect and mammalian perspectives. Archives of Insect Biochemistry and Physiology, 29, 119–134.
Bollero, D., Stella, M., Rivolin, A et al (2001). Fig leaf tanning lotion and sun-related burns: Case reports. Burns, 27, 777–779. http://doi.org/10.1016/S0305-4179(01)00033-X
Bruni, R., Barreca, D., Protti, M. et al (2019). Botanical sources, chemistry, analysis, and biological activity of furanocoumarins of pharmaceutical interest. Molecules, 24(11), 1–25. https://doi.org/10.3390/molecules24112163
Chan, J. C. Y., Sullivan, P. J., O’Sullivan, M. J., & Eadie, P. A. (2011). Full thickness burn caused by exposure to giant hogweed: Delayed presentation, histological features and surgical management. Journal of Plastic, Reconstructive and Aesthetic Surgery, 64(1), 128–130. http://doi.org/10.1016/j.bjps.2010.03.030
Cordoba, S., Gonzalez, C., Martinez-Moran, C. et al (2017). Bullous phytophotodermatitis caused by an esoteric remedy. Actas Dermo-Sifiliográficas, 108(1), 79–81.
De Almeida Jr., H. L., Sotto, M. N., De Castro, L. A. S. et al (2008). Transmission electron microscopy of the preclinical phase of experimental phytophotodermatitis. Clinics, 63(3), 371–37
Freund E. (1916). Uber bisher noch nicht beschriebene künstliche Hautverfärbungen. Dermatologische Wochenschrift, 63, 931-933.
Hung, W. L., Suh, J. H., & Wang, Y. (2017). Chemistry and health effects of furanocoumarins in grapefruit. Journal of Food and Drug Analysis, 25(1), 71–83. https://doi.org/10.1016/j.jfda.2016.11.008
Jensen T, Hansen KG. (1939). Active spectral range for phytogenic photodermatosis produced by Pastinaca sativa. Archives of Dermatology & Syphilis. 40, 566-577.
Klaber R. (1942). Phyto-photo-dermatitis. British Journal of Dermatology. 54, 193-211.
Kuske H. (1938). Experimentelle untersuchungen zur photosensibilisierung der haut durch pflanzliche wirkstoffe. I. Lichtsensibilisierung durch furocoumarine als ursache verschiedener phytogene dermatosen. Archiv Dermatologie und Syphilis, 178, 112-123
Lagey, K., Duinslaeger, L., & Vanderkelen, A. (1995). Burns induced by plants. Burns, 21(7), 542–543. http://doi.org/10.1016/0305-4179(95)00026-8
Li, G., Xiang, S., Pan, Y. et al (2021). Effects of cold-pressing and hydrodistillation on the active non-volatile components in lemon essential oil and the effects of the resulting oils on aging-related oxidative stress in mice. Frontiers in Nutrition, 8(June), 1–15. https://doi.org/10.3389/fnut.2021.689094
Liang, Y., Xie, L., Liu, K. et al (2021). Bergapten: A review of its pharmacology, pharmacokinetics, and toxicity. Phytotherapy Research, 35(11), 6131–6147. https://doi.org/10.1002/ptr.7221
Ljunggren, B. (1990). Severe phototoxic burn following celery ingestion. Archives of Dermatology, 126, 1334–1336.
Moreira, A. I. D., Leite, I., Guedes, R. et al (2010). Phytophotodermatitis: an occupational and recreational skin disease. Revista Da Associação Médica Brasileira, 56(3), 269–70. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20676531
Musajo, L., Bordin, F., Caporale, G. et al (1967). Photoreactions at 3655Å between pyrimidine bases and skin‐photosensitizing furocoumarins. Photochemistry and Photobiology, 6(10), 711–719. https://doi.org/10.1111/j.1751-1097.1967.tb08736.x
Pedersen, N. B., & Arlés, U. B. P. (1998). Phototoxic reaction to parsnip and UV-A sunbed. Contact Dermatitis, 39(2), 97. http://doi.org/10.1111/j.1600-0536.1998.tb05851.x
Puig, L., Moragas, J. M. (1994). Enhancement of PUVA phototoxic effects following celery ingestion: cool broth can also burn. Archives of Dernatology, 130, 809–810.
Quetglas-Llabrés, M. M., Quispe, C., Herrera-Bravo, J. et al (2022). Pharmacological properties of bergapten: Mechanistic and therapeutic aspects. Oxidative Medicine and Cellular Longevity, 2022(September 2021). https://doi.org/10.1155/2022/8615242
SCCNFP (2000). Opinion of the Scientific Committee on Cosmetic Products and Non-Food Products intended for consumers concerning furocoumarins in sun protection and bronzing products. 9th December 2003. SCCNFP/0765/03
Seligman, P. J., Mathias, C. G. T., O’Malley, M. A. et al (1987). Phytophotodermatitis from celery among grocery store workers. Archive of Dermatology, 123(11), 1478–1482. http://doi.org/10.1001/archderm.1987.01660350078017
Sforza, M., Andjelkov, K., & Zaccheddu, R. (2013). Severe burn on 81% of body surface after sun tanning. Turkish Journal of Trauma & Emergency Surgery, 19(4), 383–384. http://doi.org/10.5505/tjtes.2013.44522
Son, J., Jin, H., You, H. et al (2017). Five cases of phytophotodermatitis caused by fig leaves and relevant literature review. Annals of Dermatology, 29(1), 86–90.
Stowers J.J. (1897). Dermatological society of Great Britain and Ireland. Report of the annual meeting. British Journal of Dermatology & Syphilis, 9, 275-285.
Tisserand & Balazs (1995). Essential Oil Safety. Churchill Livingstone, Edinburgh.
Tisserand & Young (2014). Essential Oil Safety 2e. Churchill Livingstone, Edinburgh.
White, J.C. (1897). Notes on dermatitis venenata. Boston Medical & Surgical Journal, 136, 177-179
Zaynoun, S.T., Johnson, B.E., Frain-Bell, W. (1977) A study of bergamot oil and its importance as a phototoxic agent. Contact Dermatitis 3, 225-239.




Thank you for this complete information guide on such a crucial subject, which is phototoxicity. I still have a question, though: and what about room sprays with bergamot oil, do we have to follow that same table of maximum concentrations or is there another one with different specification on IFRA?
Hi Steff,
The guidelines apply for any product that is applied to the skin.