The single chemical approach
Since I became involved in aromatherapy 45 years ago, the dynamic between conventional medicine and aromatherapy has changed. Some of the weaknesses of conventional medicine (a $400 billion industry in the USA, and worth $1 trillion globally in 2014) have become more apparent, while at the same time essential oil research is validating many previously suspected properties of essential oils, as well as opening new doors for possible therapeutic action. And, essential oils are more widely used than ever before.
The single-chemical drug approach has helped to minimize the impact of many diseases, and has saved millions of lives. Pharmaceutical medications are sometimes very effective, and often benefits outweigh risks. But other times the risks seem worse than the benefits, or the medication simply does not work. ADRs (adverse drug reactions) are responsible for an estimated 106,000 deaths in the USA annually (statistics now 10 years old). The increasing widespread use of medication, and of medical intervention, has generated its own set of problems.
 Rob Dunn writes, in The Wild Life of Our Bodies: “…just as we seem to be getting better at ridding ourselves of the old threats, a set of “new diseases”—including Crohn’s, inflammatory bowel disease, rheumatoid arthritis, lupus, diabetes, multiple sclerosis, schizophrenia and autism, among others—has become more and more common and these diseases…have become most common precisely in those countries where we spend the most on health care and public health.” One aspect of the proliferation of ‘healthcare’ is that, increasingly, bacteria are becoming resistant to antibiotics. It’s a massive, escalating problem.
Rob Dunn writes, in The Wild Life of Our Bodies: “…just as we seem to be getting better at ridding ourselves of the old threats, a set of “new diseases”—including Crohn’s, inflammatory bowel disease, rheumatoid arthritis, lupus, diabetes, multiple sclerosis, schizophrenia and autism, among others—has become more and more common and these diseases…have become most common precisely in those countries where we spend the most on health care and public health.” One aspect of the proliferation of ‘healthcare’ is that, increasingly, bacteria are becoming resistant to antibiotics. It’s a massive, escalating problem.
It seems to be a truism that if you repeatedly try to kill something with a single substance, eventually the ‘something’ will develop resistance. We see this not only in bacteria, but also in fungi, arthropods (insects, lice, ticks, mites) and cancer cells. It is the principal reason for the corresponding failure of many antibiotic drugs, antifungal drugs, insect repellents and head lice treatments. It is the reason that most chemotherapy protocols now employ more than one drug, and frequently three or four at the same time – single drugs no longer work, because cancer cells have developed resistance to them.
“If you repeatedly try to kill something with a single substance, eventually the ‘something’ will develop resistance”
The resistance problem
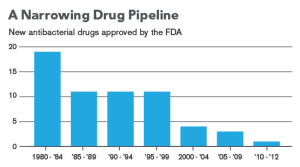
The progress of resistance has happened much faster than it might have done because of antibiotic over-use – both in medicine and farming. Incredibly, this issue has been know about for the past 50 years, and as yet there is no viable solution. In 2014 the WHO reported that, globally, 700,000 people die from antibiotic-resistant infections every year (most of them ‘nosocomial’ – acquired in hospital). Resistance to almost all antibiotics is escalating, and no new antibiotic drugs are being developed. Unless something changes, we could see 10 million more deaths a year worldwide by 2050. Drug resistant E. coli, malaria and tuberculosis would have the biggest impact.
A significant weakness in our ‘healthcare’ system is that we are now seeing the very serious downside of the widespread use of broad-spectrum antibiotics (anti-biotic: against-life). Killing all known germs is a thoroughly bad idea to begin with, and doing so in our own bodies has had the unfortunate (but with hindsight, perhaps inevitable) consequence of creating super-bugs that are resistant to many, and in some cases, all currently used antibiotics. The term “multi-drug resistant” is self-explanatory. Incredibly, problem of antibiotic resistance has been recognized since the 1950s. The conclusion, “Antibiotics should not be used except in cases of absolute necessity” comes from an international conference in Naples in 1961. We have known about this problem for more than 50 years, and so far, no solution has been found. Why? Because until very recently, conventional thinking followed the usual path – if there’s a disease, the pharmaceutical companies will develop drugs to combat it. If old antibiotics no longer work, well then they will develop new ones. There are two distinct problems with this notion.
1) The cost of new drug development is privately funded. Unless pharmaceutical companies envisage major profits they won’t invest, and antibiotics don’t excite shareholders. Two million infections per year in the USA may sound like a lot, but most patients only take a course of antibiotics once every few years. This cannot compare to a drug that is taken daily, long-term. Tellingly, there are no antibiotics in the top 100 drugs sold in the USA in 2014. Governments have tried to circumvent this problem by offering financial incentives for new antibiotic development. But so far, no one is very interested.
2) Bacteria have seen this movie before, they outnumber us, and in some ways they are us. Numerically, we are 10% human and 90% bacterial, though in terms of mass, we are still mostly human. There are estimated to be five million trillion trillion bacteria on planet earth. The worldwide bacterial biomass is greater than that of all plants and animals combined, and they have been here for about 3 billion years. That’s a long time to learn survival techniques.
 Antibiotics are used in farming as “growth promoters”. Intensive animal farming often means keeping pigs or chickens in enclosed spaces, and the lack of movement, combined with psychological stress, often leads to poor immunity and weak animals. For reasons that are not fully understood, giving these animals antibiotics increases muscle mass, and so is cost-effective for the farmer. However, this also breeds antibiotic-resistant bacteria into our ecosystem, and eating the meat produced in this way is just one of the routes by which these bacteria find their way into our own bodies. Now, essential oils are increasingly used instead of antibiotics as growth promoters, and this has become one of the most thriving areas of essential oil research.
Antibiotics are used in farming as “growth promoters”. Intensive animal farming often means keeping pigs or chickens in enclosed spaces, and the lack of movement, combined with psychological stress, often leads to poor immunity and weak animals. For reasons that are not fully understood, giving these animals antibiotics increases muscle mass, and so is cost-effective for the farmer. However, this also breeds antibiotic-resistant bacteria into our ecosystem, and eating the meat produced in this way is just one of the routes by which these bacteria find their way into our own bodies. Now, essential oils are increasingly used instead of antibiotics as growth promoters, and this has become one of the most thriving areas of essential oil research.
The statistics are worrying. According to the World Health Organization (WHO), 7% of hospitalized patients in developed countries will acquire at least one healthcare-associated infection (HAI) – an infection acquired in hospital. The figure for developing countries is 10%. In high-income countries, 30% of patients in an intensive care unit (ICU) are affected by at least one HAI. A common reason for these infections is that they are “device-associated” (DA-HAI), meaning that the source of infection is a central line, urinary catheter, stent, ventilator or other medical device. Bacterial resistance to antibiotics in DA-HAI patients is very high. In pooled data from 36 countries (gathered 2004-2009) 66.7% of patients with a central line had E. coli infections resistant to ceftriaxone or ceftedizime, 76.3% had K. pneumonia infections resistant to the same two antibiotics, and 84.4% had S. aureus infections resistant to oxacillin (Rosenthal et al 2012). Every year in the USA, two million patients contract infections in hospitals, and an estimated 103,000 die as a result. Of these, 23,000 die from bacterial infections that are resistant to antibiotic treatment. World-wide fatalities from antibiotic-resistant infections (most of them in hospitals) are estimated to be 700,000.
These deaths are regrettable and shocking. They are a direct result of antibiotic over-use, combined with hospital protocols for hand hygiene that either no longer work or are not adhered to by over-worked hospital staff. Bacteria are now developing resistance to the very substances used in hospital hand hygiene products – mostly chlorhexidine and triclosan. The problem with triclosan has been a classic case history in bacterial resistance, and in 2014 the FDA questioned its use in consumer hand hygiene products. It now seems likely that essential oil-based hand hygiene could provide a viable alternative for hospital use, thus potentially saving lives. In their review of the synergy between essential oil components and antibiotics, Langeveld et al (2013) conclude: “A topical application of EOs is most easily envisioned, and could contribute to a reduction in antibiotic use for infections.” They also add that “use of EOs systemically, although challenging, should not be ruled out as a future application.”
Essential Oils
Bacteria were first observed in 1632 by Antonie van Leeuwenhoek, who called them “animalcules”, but the connection between bacteria and infection was not made until the 1860s, notably by Louis Pasteur. This lead to the use of antiseptics during surgery, championed by British surgeon Joseph Lister in 1867, and one of the early antiseptics was named after him. The formula for Listerine has hardly changed in almost 150 years, though it is no longer used as a surgical antiseptic. The active ingredients are four essential oil constituents, menthol, cineole, thymol and methyl salicylate. Both thyme oil and eucalyptus oil were used as surgical antiseptics by some doctors in the 1880s (Lawrie 1882) and eucalyptus oil was used for respiratory infections (Murray-Gibbes 1883). The antimicrobial (antibacterial and antifungal) power of essential oils has been researched since 1887, when Charles Chamberland, who worked with Pasteur, noted that oils of cinnamon bark, oregano and geranium were active against Bacillus anthracis.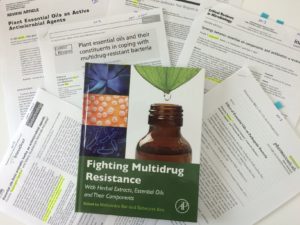
Many essential oils are quite potent antibacterial agents, and they are increasingly used in food packaging for that very reason (Burt 2004, Vergis et al 2013). There is a growing consensus that they offer one possible solution to the problem of bacterial resistance. Essential oils that effectively inhibit both methicillin-resistant Staphylococcus (MRSA) and vancomycin-resistant Enterococus (VRE) include tea tree, thyme, peppermint, lemongrass and geranium (Carson 1995, Doran 2009, Nelson 1997).
“The fact that they can sometimes reverse antibiotic
resistance in bacteria is seemingly miraculous”
Essential oils look like a good option for a number of reasons. Pathogenic bacteria are not becoming resistant to them, partly because essential oils can sometimes reverse resistance in bacteria – turn it off – and partly because they can effectively inhibit bacterial communication. This means that bacteria don’t become virulent and aggressive, even though they are not eliminated. I love the idea that essential oils are not only calming to humans, but to bacteria as well.
So far, the weight of evidence suggests that bacteria do not develop resistance to essential oils. It could happen, and we should not make the mistake of underestimating nature, but a consensus of opinion is emerging that the complexity of essential oils, and the fact that they target disease-causing bacteria in multiple ways, makes them as close to resistance-proof as it’s possible to be. This makes sense when we remember that one reason for plants creating essential oils is to guard against microbial infection, and that these oils have been evolving for millions of years for this very purpose.
Resistance in bacteria to antibiotics generally happens through genetic mutations that are passed rapidly to other bacteria. However “…it is difficult to envisage a single genetic mutation or series of mutations that would render microbial membranes impervious to essential oils yet allow normal cell functioning. Any potential mutations to membrane properties that confer resistance to essential oils are likely to also negatively impact general microbial growth and survival.” (Hammer & Carson 2011). If resistance to essential oils does become a problem in future, the over-exposure to essential oils often promoted by multi-level marketing companies may, with hindsight, look like bad move for humankind.
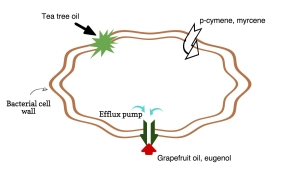
The fact that essential oils can kill bacteria that are resistant to antibiotics is amazing in itself. The fact that they can sometimes reverse antibiotic resistance in bacteria is seemingly miraculous. The most tested mechanism is in something called an efflux pump. This is a “channel” in the bacterial cell wall that spits out an antibiotic before it has time to fatally damage the cell. Both grapefruit oil and eugenol (the major constituent of clove oil) have been shown to turn off efflux pumps in some bacteria, thus removing their resistance to antibiotics (see illustration). Further mechanisms include that of p-cymene and myrcene, which have little actual antibacterial effect, but vastly aid the absorption into the bacteria of other substances, such as antibiotics, or other essential oil constituents. These mechanisms are discussed by Langeveld et al (2013).
Bacterial communication
Just as importantly, essential oils don’t just ‘kill’ bacteria; they interfere with a bacterial communication system known as “quorum sensing” (QS) and this stops bacteria becoming virulent. “Virulence” here includes swarming (multiplying rapidly) biofilm formation, and the secretion of bacterial toxins. When bacteria are ‘quiescent’ they often do not pose a threat to health, even though they have not been eliminated. QS was discovered by Dr. Bonnie Bassler, and you can see her TED talk about it here. QS is mentioned by Dr. Ramanan Laxminarayan as one of several alternatives to traditional antibiotics at 11.30 in The Coming Crisis in Antibiotics. The “antiquorum sensing activity” of essential oils is discussed in a review by Nazzaro et al 2013 on the effect of essential oils on disease-causing bacteria.
“I really do think we’re on to something here.”
The future
This all sounds great for the possible use of essential oils to either replace antibiotics or be used alongside them, but there is very little clinical research. However, developments in farming suggest interesting possibilities. In a January 2015 blog post, Tina Rodriguez of The Atlantic writes: Researchers have directly compared the effects of commonly used antibiotics with those of various essential oils. One such study, from the March 2012 issue of the Journal of Animal Science, found that rosemary and oregano oils resulted in the same amount of growth in chickens as the antibiotic avilamycin, and that the oils killed bacteria, too. Additional findings have shown that essential oils help reduce salmonella in chickens, and another study found that a blend of several oils can limit the spread of salmonella among animals. One of the co-authors of that study, Dr. Charles Hofacre, a professor at the University of Georgia’s College of Veterinary Medicine, says it’s such a new area of research that they don’t yet know exactly how the essential oils work, but “there is some strong evidence that they are functioning by both an antibacterial action in the intestine and also some have an effect to stimulate the intestinal cells ability to recover from disease more quickly–either by local immunity or helping keep the intestinal cells themselves healthier.”
 This kind of research is not going unnoticed, and essential oils are increasingly being used in animal farming instead of antibiotics. Tina Rodriguez again: One farmer who has talked publicly about using essential oils is Scott Sechler, owner of Bell & Evans Farms, a high-end producer of antibiotic-free poultry. Back in 2012, he told the New York Times about his use of oregano oil and cinnamon to fight infection on his farms, which now number about 140 with a total of 9 million chickens at any given time. Though he says the approach worked better than all other options he had tried, he still told the Times, “I have worried a bit about how I’m going to sound talking about this,” adding, “But I really do think we’re on to something here.”
This kind of research is not going unnoticed, and essential oils are increasingly being used in animal farming instead of antibiotics. Tina Rodriguez again: One farmer who has talked publicly about using essential oils is Scott Sechler, owner of Bell & Evans Farms, a high-end producer of antibiotic-free poultry. Back in 2012, he told the New York Times about his use of oregano oil and cinnamon to fight infection on his farms, which now number about 140 with a total of 9 million chickens at any given time. Though he says the approach worked better than all other options he had tried, he still told the Times, “I have worried a bit about how I’m going to sound talking about this,” adding, “But I really do think we’re on to something here.”
Looking at the future possibilities for humans, Kon and Rai (2012) write: “The complexity of essential oils is their advantage and disadvantage simultaneously. Multicomponent composition gives benefit in overcoming bacterial resistance; however, at the same time, this creates problems with standardization of EOs as medical preparations and slows their scientific and practical implementation.” This contrasts with the view of Dr. D’Angelo, who developed an antibacterial tablet based on essential oils, and says that he intentionally varies the relative proportions of the essential oils in the product, in order to minimize the risk of resistance.
With the conventional view that single-chemical drugs are the way to go, there is a risk that single essential oil constituents will be used in drug development, and will give rise to resistance. However, the thinking is starting to change. Complexity and synergy are no longer dirty words. There is hope.
References and further reading
Boire, N. A. (2013). Essential Oils and Future Antibiotics: New Weapons against Emerging “Superbugs”? Journal of Ancient Diseases & Preventive Remedies, 01(2), 1–5.
Burt, S. (2004). Essential oils: Their antibacterial properties and potential applications in foods – A review. International Journal of Food Microbiology, 94, 223–253.
Carson, C.F., Cookson, B.D., Farrely, H.D., & Riley, T.V. (1995). Susceptibility of methicillin-resistant Staphylococcus aureus to the essential oil of Melaleuca alternifolia. Journal of Antimicrobial Chemotherapy 35(3), 421-424
Doran, a L., Morden, W. E., Dunn, K., & Edwards-Jones, V. (2009). Vapour-phase activities of essential oils against antibiotic sensitive and resistant bacteria including MRSA. Letters in Applied Microbiology, 48(4), 387–92.
Faleiro, M.L., & Miguel, M. G. (2013). Use of Essential Oils and their Components against multidrug-resistant bacteria. In: Kon, M. Rai, K. (eds) Fighting Multidrug Resistance with Herbal Extracts, Essential Oils and their Components, Academic Press, Amsterdam.
Gattefossé R-M, Tisserand RB (ed.) 1993 Gattefossé’s aromatherapy: the first book on aromatherapy. CW Daniel, Saffron Walden.
Glinel, K., Thebault, P., Humblot, V., Pradier, C. M., & Jouenne, T. (2012). Antibacterial surfaces developed from bio-inspired approaches. Acta Biomaterialia, 8(5), 1670–1684.
Hammer K. A, & Carson C (2011) Antibacterial and antifungal activities of essential oils. In: Thormar, H. (ed) Lipids and Essential Oils as Antimicrobial Agents. Wiley, Chichester.
Kon, K. V., & Rai, M. K. (2012). Plant essential oils and their constituents in coping with multidrug-resistant bacteria. Expert Review of Anti-Infective Therapy, 10(7), 775–790.
Langeveld, W. T., Veldhuizen, E. J., & Burt, S. (2014). Synergy between essential oil components and antibiotics: a review. Critical Reviews in Microbiology, 40, 76–94.
Lawrie, E. (1882). Two cases of amputation treated with eucalyptus globulus. The Lancet, 12.
Murray-Gibbes, J. (1883). The blue gum steam treatment of diphteria. The Lancet, 362–364.
Nazzaro, F., Fratianni, F., De Martino, L., Coppola, R., & De Feo, V. (2013). Effect of essential oils on pathogenic bacteria. Pharmaceuticals, 6, 1451–1474.
Nelson, R. (2000). Selection of resistance to the essential oil of Melaleuca alternifolia in Staphylococcus aureus. Journal of Antimicrobial Chemotherapy, 549–550
Pauli, A., & Schilcher, H. (2004). Specific Selection of Essential Oil Compounds for Treatment of Children’s Infection Diseases. Pharmaceuticals, 1, 1–30.
Radulović, N. S., Blagojević, P. D., Stojanović-Radić, Z. Z., & Stojanović, N. M. (2013). Antimicrobial plant metabolites: structural diversity and mechanism of action. Current Medicinal Chemistry, 20, 932–52.
Ríos, J. L., & Recio, M. C. (2005). Medicinal plants and antimicrobial activity. Journal of Ethnopharmacology, 100, 80–84.
Seow, Y. X., Yeo, C. R., Chung, H. L., & Yuk, H.-G. (2014). Plant essential oils as active antimicrobial agents. Critical Reviews in Food Science and Nutrition, 54(February 2015), 625–644.
Solórzano-Santos, F., & Miranda-Novales, M. G. (2012). Essential oils from aromatic herbs as antimicrobial agents. Current Opinion in Biotechnology, 23(April 2009), 136–141.
Tabassum, N., & Vidyasagar, G. M. (2013). Antifungal investigations on plant essential oils. A review. International Journal of Pharmacy and Pharmaceutical Sciences, 5, 19–28.
Vergis, J., Gokulakrishnan, P., Agarwal, R. K., & Kumar, A. (2013). Essential Oils as Natural Food Antimicrobial Agents: A Review. Critical Reviews in Food Science and Nutrition, In Press
Yap, P. S. X., Yiap, B. C., Ping, H. C., & Lim, S. H. E. (2014). Essential oils, a new horizon in combating bacterial antibiotic resistance. The Open Microbiology Journal, 8, 6–14.


Thank you for this summary! Could you comment on the effect of the “antibiotic” essential oils on normal flora? Is the effect stronger against particular bacteria, or does it depend on the growth rate of the bacteria in the infection, or is this unstudied?
This is an issue that does need more research. Essential oils certainly will have some effect. We should think of it in terms of the “balance” of gut flora, and whether this is changed in a way that is beneficial or detrimental. Some work has been published on essential oils and gut flora in animals, especially pigs, which helps to show the range of dietary amounts of a particular EO that work well. In the meantime, here’s a post from 2014 http://roberttisserand.com/2014/07/essential-oils-gut-flora/
Hello Robert,
I am interested in using essential oils to assist with oral health issues and then repopulating my oral cavity with specific oral probiotics. Would you have a recommendation of whether the oils should be should first for a while and then followed by the probiotics to can they be used simultaneously?
Thanks for your work. I have your book, Essential Oil Safety & refer to it frequently!
Hey Robert,
Thank you for the informative article. This is such an important subject matter. I was wondering if you could weigh in on the potential for standardized oils presenting the same issue with microbial resistance. I’ve run across a companies that appear to very much be standardizing their essential oils (based on what they have said) with significant followings as well as. With their oils being used so prevalently, are we at risk of finding essential oils, at least to some extent, compromised in this matter if frequent, multiple times a day use with standardized product continues? Thank you again!
“Standardized oils” means essential oils that fall within certain standards, which include primarily ISO standards. This does not mean that an essential oil has exactly the same composition every time, since the ISO standards have quite broad ranges for each constituent. For example, the standard for menthol in peppermint oil is 32-49%, and the standard for terpinen-4-ol in tea tree oil is 30-48%. Standardized essential oils are basically no different to non-standardized oils, except that their composition conforms to the standard. On the other hand, the widespread daily use of high concentrations of essential oil – any essential oil – is a concern in terms of microbial resistance. Essential oil blends that contain highly potent antimicrobial oils may be appropriate in cases of infection, but should not be liberally used for prevention in my opinion. This, however, may conflict with business goals.
As a Registered Nurse who has observed the devastation caused by MRSA, VRE. and the like, this is a big interest in my life as I recently am working to certify in aromatherapy and wish to learn all I can. So MLM companies will not release their GC/MS and I find that disturbing also, tho I can understand a little of their hesitation, ungrounded that may be to me as I would think all consumers, and those of my like mind to learn, once educated would benefit from knowing what they are purchasing. My question to you is this: Presently in there any more ongoing research into this topic of Essential Oils to curb/assist antibiotic resistance and if so, where should I be looking? Thank you, I am learning so much!!!
Hi Jacqueline, yes, there is ongoing research into antibiotic resistance and essential oils. A good place to look for research is PubMed, https://www.ncbi.nlm.nih.gov/pubmed
Hello,
After reading Essential Oil Safety second edition over the past couple of years, I’ve recently joined your institute and discovered this post through your Foundations webinar. Synergy makes so much sense, it has to be the way forward. I’m really looking forward to the Masterclass.
Best,
Claudia
Hello folks. I’m interested in reliable sources. Is there any studies about using EOs to fight viruses? A lotta companies that produce EOs talking about it but sometimes they are trying to sell not to provide the truth, so I’m looking for some kinda independent researches about EOs vs virus. Pls share if u know anything about this specific topic. Thanks.
Viruses are very different to each other, so the term “antiviral” for an essential oil does not apply equally to all viruses. This article explores the science and application of essential oils for influenza viruses: https://tisserandinstitute.org/essential-oils-flu/
if we start using essential oils in the place of common disinfectants or antibiotics, is there a risk of bacteria developing a resistance to essential oils too? Will using varying the proportions of essential oils at once really preclude this risk in the long run?
Hi Aaron, that’s a good question, and one that we don’t yet have a definitive answer for. It does seem likely that, eventually, some bacteria will develop resistance to some essential oils, and the more widely the oils are used against bacteria, the more likely this is to happen. So I think the consensus view is to move forward in ways that may save lives, while at the same time being vigilant.