Introduction
In 2012, Posadzki, Alotaibi and Ernst published a systematic review, which “was aimed at critically evaluating the evidence regarding the adverse effects associated with aromatherapy” (Posadzki et al, 2012). However, it is an article awash with inaccuracy and offers a text-book example of what a systematic review is not. The aim of a systematic review (SR) is to provide a high-level summary of the best available evidence, which has been systematically collated and reviewed. A goal of SR methodology is that it ‘designs out’ bias and improves rigor. The purpose of the SR is to provide the reader with a reliable, credible, accurate and complete synopsis of the evidence, based on a thorough, a priori critique of the articles under review. The results should be reliable and replicable, and the summary should inform clinical decision making and evidence-based practice (EBP). Sackett et al (1996) defined EBP as ‘the conscientious, explicit, judicious use of current best evidence in making decisions about the care of individual patients’.
Multiple critical flaws
 To ensure the current article stands up to scientific scrutiny, we reviewed the SR using a validated instrument, AMSTAR 2 (see Appendix at end of article), which measures the methodological quality of SR research (Shea et al, 2007; Smith et al, 2011). Using this instrument we determined that the article contains multiple critical flaws including:
To ensure the current article stands up to scientific scrutiny, we reviewed the SR using a validated instrument, AMSTAR 2 (see Appendix at end of article), which measures the methodological quality of SR research (Shea et al, 2007; Smith et al, 2011). Using this instrument we determined that the article contains multiple critical flaws including:
- Lack of published protocol
- Lack of assessment of risk of bias
- No consideration of risk of the bias when interpreting the results of the review
- No assessment of the presence and likely impact of publication bias
Confidence in the results of an SR is considered critically low if there is more than one critical flaw, and the results “should not be relied on to provide an accurate and comprehensive summary of the available studies” (Shea et al, 2017). Further, where the authors have reported criteria (patient population, non-cosmetic products only) they have not met their own specifications.
There are also some ‘non-critical weaknesses’ including the lack of questions based on Population, Intervention, Comparison and Outcome (PICO) see image at right. Both critical and non-critical flaws are discussed in further detail, below.
The aim of the systematic review
The stated aim of the Posadzki et al systematic review was to “provide a summary and critical evaluation of the evidence regarding adverse events (AEs) associated with the use of aromatherapy”. As with all published research, transparency of the intention of the authors helps the reader to determine the reliability of the findings. No statement or explanation is provided of specifically what evidence regarding AEs will be summarised or critically evaluated. Immediately after stating the Aim, the authors go on to describe in the Method section that this exercise was limited to “case series (CS) and case reports (CR) of AEs of aromatherapy in human patients” (a ‘case series’ is a report on several related cases).
 Case series and case reports provide clinicians and researchers with some knowledge, alerting them to incidences that have occurred. When compiled they may generate clinical questions for systematic reviews, and often these observations facilitate further research. However, they are descriptive and are often an incomplete reporting of rare events; to generalize to the whole population is problematic. As the basis of a systematic review, they should not be the final word on a topic, unless the findings are further synthesised with published best evidence, e.g. from randomised controlled trials, rigorous systematic reviews, and meta-analyses. For example, there are numerous reports in the literature comparing the incidence of reactions by dermatology patients to patch testing with various essential oils (Tisserand & Young 2014 p388). Since Posadzki et al have not cited any of this research, their conclusion that peppermint is one of the most likely essential oils to cause an adverse reaction is wrong and misleading.
Case series and case reports provide clinicians and researchers with some knowledge, alerting them to incidences that have occurred. When compiled they may generate clinical questions for systematic reviews, and often these observations facilitate further research. However, they are descriptive and are often an incomplete reporting of rare events; to generalize to the whole population is problematic. As the basis of a systematic review, they should not be the final word on a topic, unless the findings are further synthesised with published best evidence, e.g. from randomised controlled trials, rigorous systematic reviews, and meta-analyses. For example, there are numerous reports in the literature comparing the incidence of reactions by dermatology patients to patch testing with various essential oils (Tisserand & Young 2014 p388). Since Posadzki et al have not cited any of this research, their conclusion that peppermint is one of the most likely essential oils to cause an adverse reaction is wrong and misleading.
The authors decided to exclude data from clinical trials. The decision to exclude randomized controlled trials (RCTs) and to only include low-level evidence does not have a reasonable basis. In a 2012 systematic review looking only at chiropractic manipulations, Ernst and Posadzki (2012) reported that “clinical trials of alternative therapies fail to report AEs”. This is a very weak argument to justify the exclusion of a larger body of higher quality evidence regarding aromatherapy treatments.
The systematic review should answer a specific, clinical question. In this case, the authors provide no research question, or justification for their review. The question should indicate a clinical issue to be analyzed or challenged (Aslam and Emmanuel, 2010), and justification adds credibility to the research. The title of the SR “adverse events in aromatherapy” is vague, and not a true representation of the content. While the authors have provided a definition of aromatherapy, “the controlled use of plant essences for therapeutic purposes” (Ernst et al, 2006), they have failed to include even a single case study that falls within this definition. “Plant essences” is not a defined term, either in the systematic review, or anywhere else. It could mean ‘essential oil’, but it could also mean a water infusion for example.
“Aromatherapy is the therapeutic use of essential oils” (Buckle, 2008). An essential oil is a product obtained from a natural raw material of plant origin, by steam distillation (which includes hydrodistillation), by mechanical processes from the pericarp (peel) of citrus fruits, or by dry distillation, after separation of the aqueous phase -if any- by physical processes (International Organization for Standardization, 2013). The therapeutic application of essential oils includes topical (skin) application, inhalation, or oral routes (although the latter is generally accepted as a form of herbal medicine) (Buckle, 2008).
The search strategy
The authors described their search strategy in some detail, providing a list of key search terms, and detailing the databases in which they conducted their search, allowing the reader to replicate it. However, they have not detailed the period of time included in their search strategy, and this is necessary for future researchers who may want to build on the evidence provided by a single SR.
The identification of articles for the systematic review was done in consultation with at least two authors but these authors are not identified. ‘Any disagreements were resolved through discussion’ and based on ‘pre-defined criteria’ (Posadzki et al, 2012) but the criteria are not given. Exclusion criteria include accidental ingestion of essential oil (EO), and EO as an ingredient in food, fragrance, or cosmetic production.
Results of the search
The authors cite a total of 71 cases, including several cases of practitioner contact dermatitis. Contact dermatitis is the skin’s response to an allergen or toxin. It should be noted that up to 70% hairdressers experience contact dermatitis because of their work (Ford, 2012). These adverse events are occupational hazards, and protocols are put in place to reduce the risks. For example, an aromatherapist may exclude an essential oil from their practice to reduce the risk of triggering or exacerbating a previous reaction.
It is not clear why the authors included articles describing adverse events that do not fall either within the practice of aromatherapy, or within their own inclusion criteria. For example, one study reports on “recurrent allergic contact dermatitis due to allergen transfer by sunglasses” (Williams et al 2007). Another describes the application of a balm containing camphor, followed by ‘cao giao’, a Cambodian traditional medicine practice in which the skin is vigorously rubbed with coins (Rampini et al 2002); this is not current aromatherapy practice. Based on the exclusion criteria defined by the authors, adverse events occurring after accidental ingestion of oils or the application of personal care products such as hair gel and shampoo should not have been included.
Three reports are included that involve accidental poisoning, one fatal. The fatal report concerns an 80-year-old man with end-stage renal (untreatable kidney) disease. In this case report, a live-in attendant had applied oil of wintergreen, stated as containing 35% mg/mL methyl salicylate, to the gentleman’s legs on a regular basis (regular is not quantified). The attendant left the bottle on the nightstand, and the man mistook it for a drink, and accidentally consumed “a mouthful” (Chin, Olsen and Dempsy, 2007). These details are omitted from the systematic review. Had they been reported, it would have been obvious that the case report met the exclusion criteria and that it should not have been included in the review.
It is not clear from either the systematic review nor the original case study whether the product was wintergreen oil, or diluted methyl salicylate. Wintergreen oil contains 97-99% methyl salicylate, not 35% (35% mg/mL makes no sense, as 35 mg/mL is equivalent to 3.5%). This is important when it comes to the reporting of death due to a product. Many commercial products are made with a 30% or 35% dilution of synthetic methyl salicylate, and this information should inform commercial manufacturers about the dangers which may be associated with this ingredient in their products. The reporting of the ingredient that ultimately ended this man’s life would provide concrete evidence of whether this was an essential oil, or not. Either way, this was clearly a case of accidental poisoning, in a man, who was close to death.
Accidental ingestion is certainly not aromatherapy. Nevertheless, the systematic report has been cited numerous times to support statements suggesting “death” as a possible outcome of aromatherapy in (Owen & Laird, 2018; Priyah et al, 2018; Rad et al, 2017; Dagli et al, 2015; Githae-Jansson, 2014; Stea et al 2014; Fonareva, 2013) and on the world wide web (RationalWiki 2018).
Two of the reported cases were injuries resulting in skin grafts. The first was a workplace injury where a pharmaceutical manufacturing employee accidentally spilled undiluted peppermint oil onto a previous burn injury (not by essential oils) (Parys 1983). The second describes full thickness skin and tissue necrosis following the application of a gel containing 30% methyl salicylate and 11% menthol. The patient then covered with a heat pad, “despite manufacturers warnings against the use of heating pads” (Heng 1987). Both cases fall outside aromatherapy practice.
The authors of the SR have estimated causality; however, they have not reported the criteria for this determination. The establishment of causality (the relationship between cause and effect) requires demonstrating association (time/place), temporal precedence (the direction of influence), non-spuriousness (there can be no other possible contributing variables), medical plausibility (tested, not assumed) and what happens after the treatment has ended (WHO, 2012).
In all the cases listed in the SR, the authors have made estimates based on the application of the product and direction of influence. However, they have not proven ‘non-spuriousness’. Therefore, their conclusions are not supported. One article describes a potential interaction between essential oils and anti-fungal medication (Varma, 2000). Another describes the case of the six-year-old child whose parents applied a concoction of up to 50 ml of eucalyptus oil, apple cider vinegar, olive oil and methylated spirits (95% ethanol, no methanol), followed by occlusion with cling film, based on advice they received from a talk radio program (Darben et al, 1998).
Despite the criteria to exclude case studies reporting AEs associated with cosmetic products, the authors have included three: “Use of a neroli oil facial moisturizer” (Newsham et al 2011); the daily application of commercially available styling gel and shampoo (Henley et al 2007); and the “use of lavender-scented soap and intermittent use of lavender-scented commercial skin lotions” (Henley et al 2007). By the authors own criteria, these articles should not be included in this SR; they are clearly not part of aromatherapy practice, and the adverse events are an issue for the commercial manufacturers.
The authors show their lack of understanding of the subject matter by including four reports that concern fatty oils and not essential oils. These are black seed oil (Nosbaum et al 2011), mustard seed oil (Zawar 2005), neem oil (Greenblatt et al 2011), and tamanu oil (Le Coz 2004). Black seed and mustard also exist as essential oils, but these papers concern the fatty oils, although one of them states “essential oil” in the title. The chemical composition of fatty oils – mostly non-volatile fatty acids – is completely different from the volatile constituents of essential oils. Since biological activity, including adverse effects, will depend on the chemical composition of the oils, the difference is crucial. From the inclusion of adverse events associated with the use of fatty oils, it is clear the authors do not appreciate the distinction.
Risk of bias
Bias is a deviation from the true results, and assessment of the risk of bias helps the reader estimate the weight (significance) that may be ascribed to the outcomes (conclusions). One example of this may be consistent results across studies, but flawed methodology in one or more trials. For example, the study sample may not be adequate, or the design may not reflect real world practice (testing something against nothing, rather than testing against current best practice). As the authors have not stated a specific question they wish to answer, it is difficult to assess bias in this study. This is a significant flaw of their systematic review.
The author conclusions
The lack of a defined scientific objective of the systematic review and the inclusion of articles meeting the exclusion criteria, combined with other methodological flaws, seriously undermine the legitimacy of the conclusions drawn by the authors.
The authors reported the following four main conclusions:
- “In conclusion, aromatherapy has the potential to cause AEs which can occasionally be serious.”
Identifying the potential risk of adverse events was not a stated aim. Nor was defining the occurrence of serious adverse events or the spectrum of severity. No definition is given for “serious” adverse events. It is also worth noting that any substance taken as a medicine, whether drug, dietary supplement, herb or essential oil, has the potential to cause AEs. This fact, however, should not completely invalidate the use of those substances. - “Their frequency remains unknown.”
Determining the frequency was not a stated aim of the work and was never going to be identified by looking at case reports or case series. - “Lack of sufficiently convincing evidence regarding the effectiveness of aromatherapy combined with its potential to cause AEs questions the usefulness of this CAM modality in any condition.”
The authors did not set out to identify or evaluate evidence regarding the effectiveness of aromatherapy. It was not a stated aim, effectiveness was not evaluated in any way, and therefore conclusions about effectiveness are not relevant here. While some of the risks of essential oils exposure may have been identified by the review, they were not all associated with aromatherapy, and none were associated with aromatherapy practice involving a practitioner and a patient. Weighing benefit and risk was also not a stated aim, and would not anyway be possible by simply looking at a handful of case reports or case series. - “It is questionable whether the benefits of aromatherapy outweigh its risks.”
The data in the SR do not support this conclusion as the review does not provide any measures of either the risks or the benefits of aromatherapy. This conclusion, along with the previous one, is attempt to use the SR as evidence that that aromatherapy is not effective.
The data provided in the SR do not support most of the authors’ conclusions.
Discussion
So far, we have reported on the substantial number of flaws present in the Posadzki et al article. It is fair to say that there is very little quality evidence presented by the authors, and in fact their conclusions could be quite damaging. Systematic reviews are more than a summary of the published ‘evidence’. Their purpose is to scrutinise and offer clinically and statistically meaningful conclusions. This SR is misleading: it is not transparent; it does not include all the published, high-level evidence, and the findings may be misinterpreted.
The authors have stated that they could not locate any reports of AE associated with the use of aromatherapy as an alternative (rather than complementary) treatment and have concluded that this is an ‘under-reporting’ bias. This is confusing given they have excluded clinical research. To detect this, it would have been necessary to include studies that compare the application of essential oils to current best practice. Based on the methodology employed in this SR, the authors have not been able to provide any evidence that AEs are associated with the application of EOs in the context of aromatherapy practice, therefore, their “view” is not supported.
The authors also state that ‘aromatherapists tend to deny any risks associated with aromatherapy’. Their statement is not supported by the citation provided (Guba 2001). In his article, Guba (2001) reports concerns about generalizing findings from mouse studies to humans (different metabolic processes), and findings from laboratory as opposed to clinical research (cannot describe dosing), and he highlights problems with comparing in vitro (in glass or test tube) and in vivo (in whole living organism, often in a highly controlled environment) research. Guba does not dismiss safety concerns or valuable scientific research.
The authors also say “Some aromatherapists advise their patients to ingest EOs in addition to topical application”, citing Denise Tiran (1996). This is another case of misrepresenting the work of others. Tiran does not promote the idea of ingestion. Tiran cites two articles in which ingestion of essential oils occurred. Neither article presents details of ingestion recommended by an aromatherapist. The first is a case report of accidental eucalyptus oil poisoning and a review of the literature describing the oil as a poison (Gurr & Scroggie 1965). The second is a case series of accidental ingestion of citronella oil (Temple et al, 1991).
The aims of this SR are not clear, and the results do not answer these unclear aims in relation to practitioners, patients, and aromatherapy.
There were many opportunities, even in 2012, for the authors to delve into the issues presented in the case studies, for example, highlighting concerns about blanket promotion of ingesting essential oils for ‘healthy digestion and internal organ function’ or to ‘reduce anxious feelings’ (Monroe, 2017), or explaining why applying essential oils without clinical guidance can be problematic. There is also the concern, first raised by Denise Tiran (1996) regarding the extension of clinical practice of health professionals, who lack adequate training. In other words, there is a concern about medical professionals who are practicing outside the scope of their own practice. This was also a perfect opportunity to refer readers to the importance of safe storage of essential oils to limit the effects of oxidation, and the potential for harm (Tisserand and Young, 2014 pp 10-11). None of these opportunities were explored.
Our conclusion
The authors of the SR have rightly highlighted the common misconception that anything natural is regarded as safe. The findings do support the concerns of practicing aromatherapists that the use of essential oils without clinical consultation or based on questionable advice from unqualified aromatherapists/practitioners or even talk radio programs is potentially dangerous. That essential oils can be dangerous is not disputed. However, the article under review contains methodological flaws, inconsistencies, and misleading statements which make the conclusions unreliable. The authors have excluded data from clinical trials and have failed to distinguish between the therapeutic and cosmetic use of essential oils.
The lack of a research question, failure to adhere to the criteria set for the study, and exclusion of clinical trials makes it difficult to apply the findings to any mode of practice or population, and for any specific complaint. Highlighting random – and in some cases, rare – adverse events offers very little guidance for practitioners or consumers. This is not a systematic review; it is at best a narrative summary of adverse events as presented in single case studies, or case series, most of which have limited relevance to the practice of aromatherapy. At worst it is an example of bias aided and abetted by sloppy science.
Appendix
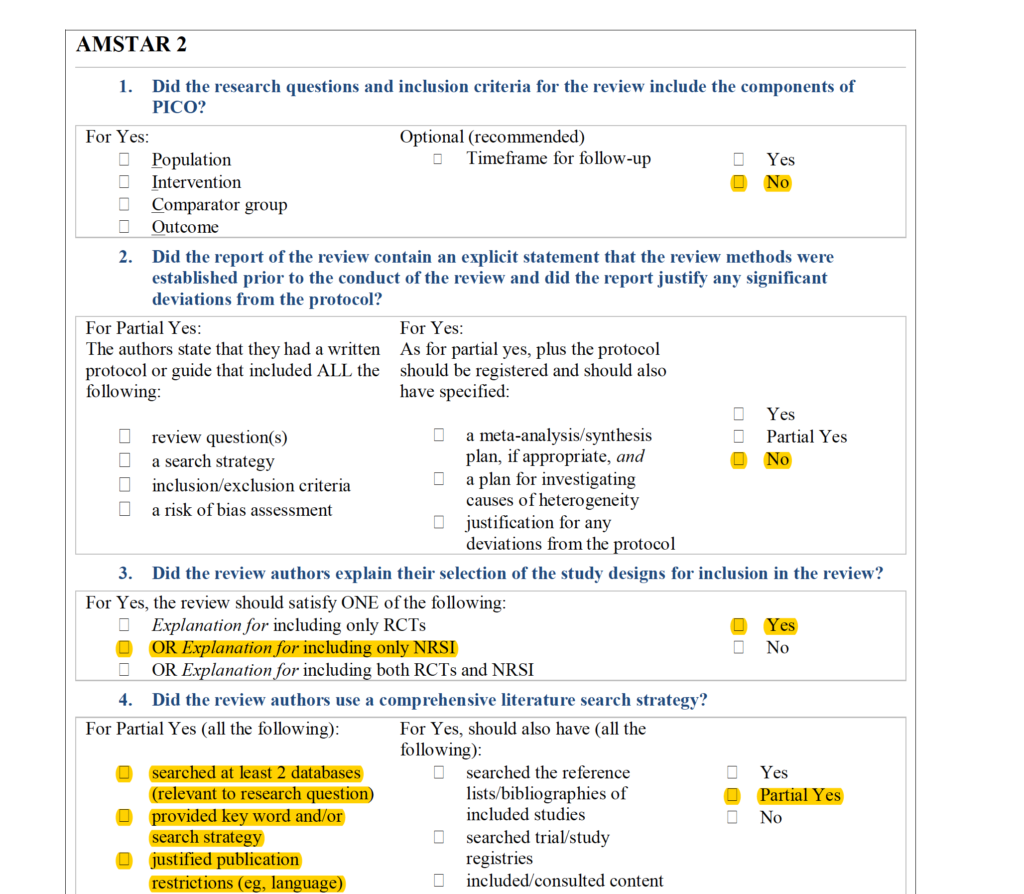
Amstar 2 assesment of the Posadzki et al article, showing that it does not meet the criteria for a systematic review. For full assessment, click the image.
References
Aslam S, Emmanuel P (2010) Formulating a researchable question: A critical step for facilitating good clinical research. Indian Journal of Sexually Transmitted Diseases, 31(1): 47-50 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3140151/
Buckle J (2008) ‘Aromatherapy’ in Freeman LW (ed) Mosby’s Complementary & Alternative Medicine: A Research-Based Approach, 3rd edn, Mosby Elsevier, St. Louis, Missouri
Chin R, Olson K, Dempsey D (2007) Salicylate toxicity from ingestion and continued dermal absorption. The California Journal of Emergency Medicine, 8(1): 23-25 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2859737/
Dagli N, Dagli R, Mahmoud RS, Baroudi K (2015) Essential oils, their therapeutic properties, and implication in dentistry: A review. Journal of International Society of Preventive & Community Dentistry, 5(5): 335-340 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606594/
Darben T, Cominos B, Lee CT (1998) Topical eucalyptus oil poisoning. Australasian Journal of Dermatology, 39: 265-267 https://www.ncbi.nlm.nih.gov/pubmed/9838728
Ernst E, Pittler MH, Wider B, Boddy K (2006) The desktop guide to complementary and alternative medicine. 2nd Edition. Edinburgh: Elsevier Mosby
Ernst E, Posadzki P (2012) Reporting of adverse effects in randomised clinical trials of chiropractic manipulations: A systematic review. New Zealand Medical Journal, 125 (1353): 87-140 https://www.nzma.org.nz/journal/read-the-journal/all-issues/2010-2019/2012/vol-125-no-1353/article-ernst
Fineout-Overholt E, Melnyk BM, Stillwell SB, Williamson KM (2010) Critical Appraisal of the Evidence: Part I – An introduction to gathering, evaluating and recording the evidence. American Journal of Nursing, 110(7): 47-52 https://www.ncbi.nlm.nih.gov/pubmed/20574204
Fonareva I (2013) Physiological, cognitive, and expectancy effects of aromatherapy following acute stress. PhD Thesis, Oregon Health & Science University, United States of America https://digitalcommons.ohsu.edu/cgi/viewcontent.cgi?article=1903&context=etd
Ford S (2012) Skin problems in hairdressers and barbers. DermNet New Zealand accessed 07/01/2018 from https://www.dermnetnz.org/topics/skin-problems-in-hairdressers-and-barbers/
Githae-Jannson C (2014) An exploration of perspectives and patterns of complementary and alternative medicine use for wellness among Finnish and Estonian people. Masters Thesis, University of Tartu, Estonia http://hdl.handle.net/10062/43450
Greenblatt DT, Banerjee P, White, JML (2012) Allergic contact dermatitis caused by neem oil. Contact Dermatitis, 67(4): 242–243. http://doi.org/10.1111/j.1600-0536.2012.02099.x
Guba R (2001) Toxicity myths – essential oils and their carcinogenic potential. International Journal of Aromatherapy, 11(2): 76-83 https://www.sciencedirect.com/science/article/pii/S0962456201800217
Gurr FW, Scroggie JG (1965) Eucalyptus oil poisoning treated by dialysis and mannitol infusion. Australasian Annals of Medicine, 14: 238-249 https://www.ncbi.nlm.nih.gov/pubmed/5862649
Heng MC (1987) Local necrosis and interstitial nephritis due to topical methyl salicylate and menthol. Cutis, 39(5): 442-444 https://www.ncbi.nlm.nih.gov/pubmed/3556044
Henley DV, Lipson N, Korach KS, Bloch CA (2007) Prepubertal gynecomastia linked to lavender and tea tree oils. The New England Journal of Medicine, 356(5): 479–485 http://doi.org/10.1056/NEJMoa064725
International Organization for Standardization (2013) 2.11 Essential Oil in Aromatic natural raw materials – Vocabulary (ISO Standard No. 9235:2013en) accessed 9 July 2018 from https://www.iso.org/obp/ui/#iso:std:iso:9235:ed-2:v1:en
Le Coz CJ (2004) Allergic contact dermatitis from tamanu oil (Calophyllum inophyllum, Calophyllum tacamahaca). Contact Dermatitis, 51(4): 216–217 http://doi.org/10.1111/j.0105-1873.2004.0424h.x
Monroe R (2017) How essential oils became the cure for our age of anxiety. The New Yorker. October 9 accessed 19 January 2018 from https://www.newyorker.com/magazine/2017/10/09/how-essential-oils-became-the-cure-for-our-age-of-anxiety
Newsham J, Rai S, Williams JDL (2011) Two cases of allergic contact dermatitis to neroli oil. British Journal of Dermatology, 165: 71–81. http://doi.org/10.1111/j.1365-2133.2011.10286.x
NHMRC (2015) How clinical trials work. Australian Government, accessed 07/01/2018 from https://www.australianclinicaltrials.gov.au/what-clinical-trial/how-clinical-trials-work
Nosbaum A, Ben Said B, Halpern S-J et al (2011) Systemic allergic contact dermatitis to black cumin essential oil expressing as generalized erythema multiforme. European Journal of Dermatology, 21(3): 447–448 http://doi.org/10.1684/ejd.2011.1350
Owen L, Laird K (2018) Synchronous application of antibiotics and essential oils: dual mechanisms of action as a potential solution to antibiotic resistance. Critical Reviews in Microbiology, 44(4): 414-435 https://www.ncbi.nlm.nih.gov/pubmed/29319372
Parys BT (1983) Chemical burns resulting from contact with peppermint oil mar: A case report. Burns, 9(5): 374–375. http://doi.org/10.1016/0305-4179(83)90087-6
Posadzki P, Alotaibi A, Ernst E (2012) Adverse effects of aromatherapy: A systematic review of case reports and case series. International Journal of Risk & Safety in Medicine, 21: 147-161 https://www.researchgate.net/publication/230768825_Adverse_effects_of_aromatherapy_A_systematic_review_of_case_reports_and_case_series
Priyah SK, Sheeba S, Ganapathy D, Kanniappan N (2018) Role of essential plant oils in the treatment of periodontal and oral diseases. Journal of Pharmacy Research, 12(1): 24-28 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606594/
Rad M, Shomoossi N, Mirhosseini Z, Kashani E (2017) Can cool dialysate alleviate restless leg syndrome in hemodialysis patients? Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences, 22: (124) http://doi.org/10.4103/jrms.JRMS_587_17
Rampini SK, Schneemann M, Retsch K, Bachli EB (2002) Camphor intoxication after cao gio (coin rubbing). JAMA, 288(1): 45 https://jamanetwork.com/journals/jama/article-abstract/1031948
RationalWiki (2018) Essential Oil, RationalWiki accessed 9 July, 2018 from https://rationalwiki.org/wiki/Essential_oil
Sackett DL et al. (1996) Evidence based medicine: what it is and what it isn’t. British Medical Journal, 312: 71-72 https://doi.org/10.1136/bmj.312.7023.71
Shea BJ, Grimshaw JM, Wells GA et al. (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology, 7(10) https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-7-10
Shea BJ, Reeves BC, Wells G, et al. (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358: doi https://doi.org/10.1136/bmj.j4008
Sheen JG, Stevens J (2002) Aromatherapy as a profession. The International Journal of Aromatherapy, 12(4): 187-192
Smith V, Devane D, Beggley CM, Clarke M (2011) Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Medical Research Methodology, 11(15) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3039637/
Statistics Solutions (2017) Establishing cause and effect. Statistics solutions accessed 22/01/2018 from http://www.statisticssolutions.com/establishing-cause-and-effect/
Stea S, Beraudi A, De Pasquale D (2014) Essential oils for complementary treatment of surgical patients: State of the art. Evidence-Based Complementary and Alternative Medicine doi.org/10.1155/2014/726341 https://www.hindawi.com/journals/ecam/2014/726341/
Temple WA, Smith NA, Beasley M (1991) Management of oil of citronella poisoning. Journal of Toxicology: Clinical Toxicology, 29(2): 257-262 https://doi.org/10.3109/15563659109038618
Tiran D, Aromatherapy in midwifery: benefits and risks (1996) Complementary Therapies in Nursing and Midwifery, 2: p88-92
Tisserand R, Young R (2014) Essential oil composition in: Essential oil safety – a guide for health care professionals 2nd edition. Elsevier, Edinburgh.
Varma S, Blackford S, Statham BN, Blackwell A (2000) Combined contact allergy to tea tree oil and lavender oil complicating chronic vulvovaginitis. Contact Dermatitis, 42(5): 309-310 https://www.ncbi.nlm.nih.gov/pubmed/10789871
WHO (2012) Safety monitoring of medical products: reporting system for the general public. Switzerland, WHO Press http://www.who.int/medicines/areas/quality_safety/safety_efficacy/ConsumerReporting.pdf?ua=1
Williams JD, Nixon RL, Lee A (2007) Recurrent allergic contact dermatitis due to allergen transfer by sunglasses. Contact Dermatitis, 57(2): 120–121. http://doi.org/10.1111/j.1600-0536.2006.01002.x
Zawar V (2005) Pityriasis rosea-like eruptions due to mustard oil application. Indian Journal of Dermatology, Venereology and Leprology, 71(4): 282-284 https://www.ncbi.nlm.nih.gov/pubmed/16394442
 Tamara Agnew, PhD, BA
Tamara Agnew, PhD, BA
Population health and research design | Australia
Tamara Agnew holds a PhD from the University of South Australia following her study on the effect of essential oils and aromatherapy on the physical and psychosocial symptoms of acne vulgaris. She is a lecturer at the University where she teaches research methods, Global National Health and First People’s Health, and she is a Research Associate at Flinders University in the Digital Health Research Centre. Tamara has developed expertise in conducting systematic reviews, clinical trials and psychometric evaluations. Tamara holds a first class honours degree from Edinburgh Napier University where she studied Complementary Healthcare (Aromatherapy). Tamara has published in multiple scientific journals and has contributed to an aromatherapy textbook, authored by Jennifer Peace Rhind. She has also reviewed articles for several journals. She is passionate about aromatherapy, integrative health care, ageing, and she has a particular interest in building the evidence base in these fields.
Robert Tisserand
Founder of the Tisserand Institute | UK, USA
Robert Tisserand is a speaker, educator and consultant on the science and benefits of essential oils and their safe and effective application, and in 1977 he wrote the first English language book on aromatherapy. In addition to teaching online courses, in recent years he has inspired live audiences in Europe, Asia, North America and South America. He was privileged to receive a Lifetime Achievement Award from the AIA in Denver in 2007, and in 2014 he co-authored the second edition of Essential Oil Safety, which has helped set industry safety standards. Robert is the principal of The Tisserand Institute.
 Christine Carson PhD
Christine Carson PhD
Microbiology, essential oil research | Australia
Christine has a PhD in Microbiology and has been investigating the biological effects of natural products, including Melaleuca alternifolia (tea tree) essential oil, for over 20 years. She has published over 50 papers in the field and is interested in the antimicrobial, anti-inflammatory and other potentially useful medicinal properties of natural products, particularly plant-derived compounds, as well as the safety and toxicity associated with their use. Christine has a broader interest in other natural products and their potential use in human health. She is a Research Associate at the University of Western Australia and the Harry Perkins Institute of Medical Research.




thank you! I have seen this ‘compilation’ quoted. Your argument will help next time. (and we all know there will be a next time.)
Excellent breakdown and thorough analysis. Thank you!