by Sue Pace
Ticks have historically been a minor annoyance and a sort of “occupational hazard” for nature lovers. Due to exponen tial growth in the number of Lyme Disease cases in recent years, tick bites are becoming a greater source of fear.
tial growth in the number of Lyme Disease cases in recent years, tick bites are becoming a greater source of fear.
Ticks are insects in the family Ixodidae and are classified as parasitic mites. While more than eight hundred species of ticks have been identifiedworldwide, approximately fifteen are known to cause disease in humans . At the beginning of their life cycle ticks do not carry pathogens (with the possible exception of Borrelia miyamoti) . They must first bite an infected animal (usually a rodent) and disease-causing organisms living inside the rodent transfer to the tick during feeding .
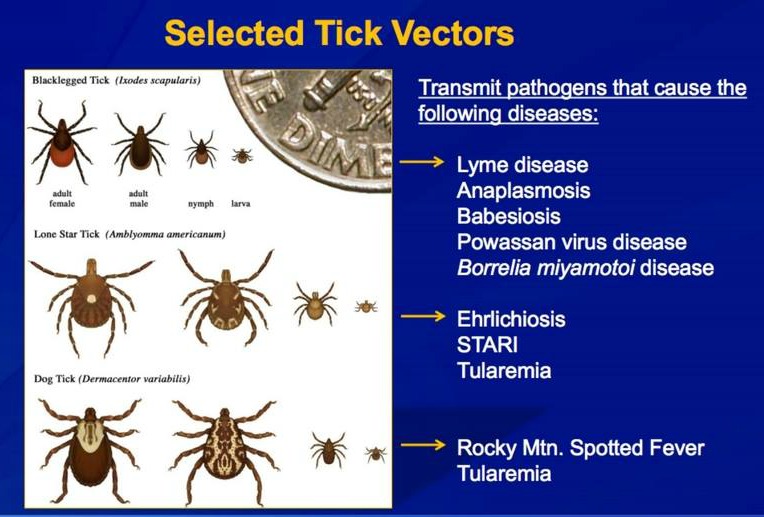
Bacteria, viruses, and microscopic protozoans are all causative agents of tick-borne illness. Some of the fifteen identified syndromes caused by infected ticks are Lyme Disease, Erlichiosis, Rocky Mountain Spotted Fever and Anaplasmosis, which are all caused by bacteria, Powassan disease, the result of infection by an arbovirus, and Babesiosis, caused by a microscopic parasite that infects the host’s red blood cells .
The scope of this article does not allow for in-depth discussion of tick-borne illnesses other than Lyme Disease, but more information about these is provided in the Box. The following graphic from the U.S. Centers for Disease Control is an excellent summation of the types of ticks known to be vectors of disease. It shows their life cycle size in relation to an American ten cent coin.
 FAQ for Lyme: https://www.cdc.gov/lyme/faq/index.html
FAQ for Lyme: https://www.cdc.gov/lyme/faq/index.html
FAQ for Powassan: https://www.cdc.gov/powassan/faqs.html
FAQ for Babesiosis: https://www.cdc.gov/parasites/babesiosis/gen_info/faqs.html
Information about Anaplasmosis
Information about Erlichiosis
Information about Rocky Mountain Spotted Fever
Lyme Disease
Lyme Disease is a well researched tick-associated illness and the one most familiar to people. The term “Lyme Arthritis” was coined in 1975 when a group of people in the Old Lyme (Connecticut) area contracted an unusual illness characterized by fatigue, fever, headache, rash, and joint pain. The illness was at first mistakenly identified as juvenile rheumatoid arthritis. Intrigued epidemiologists at nearby Yale University investigated the cluster of cases. During the investigation it became apparent that those affected had a common history of exposure to bites from the blacklegged deer tick (Ixodes scapularis). The outbreak’s location was incorporated into the syndrome’s name and in 1979 the condition was termed “Lyme Disease”. In 1982, Dr. Willy Burgdorfer of the Rocky Mountain Laboratories in Montana discovered the long-sought cause of Lyme disease, a spirochete bacterium, which was named Borrelia burgdorferi in his honor .
While it’s commonly believed that Lyme Disease is endemic only to parts of the United States, the illness is responsible for more than 300,000 estimated annual new infections in the U.S. and six of the world’s seven continents . Incredibly, blood analysis from penguins located in two sub-Antarctic islands shows evidence of antibodies against Lyme disease, the infected ticks having been transported to the remote location by migrant sea birds .
Internet searches and articles about Lyme Disease reflect a growing concern worldwide . A news story from May 18, 2017 concerning a case of “tick paralysis” in a young girl is a perfect illustration . The child’s mother posted a public Facebook video on May 13, 2017 which shows the girl struggling to stand and walk. During an Emergency Department visit, a doctor found and removed a tick in her scalp and the child has subsequently recovered. At the time of this writing, the video has garnered more than 21 million views!
How does one “get” Lyme Disease?
Lyme disease is transmitted by the bite of an infected blacklegged deer tick nymph. Pictured here magnified on the tip of a human finger, nymphs are smaller than a sesame seed and their bite is virtually painless. These factors contribute to a tick’s ability to attach itself to a host while escaping notice, and then commence feeding.
How does a tick bite?
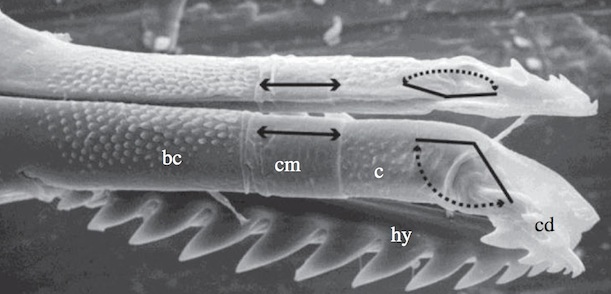
The tick’s “mouth parts” look like something out of a science fiction movie! In this image, three separate structures work together to allow the tick to bite and anchor itself in the skin. Two appendages called chelicerae (labeled “cd”) have telescoping barbs which allow them to penetrate the outer epidermis. Once attached, the tips of the chelicerae bend apart laterally in a “breast stroke” type motion, allowing the even sharper hypostome (labeled “hy”) to move between them and burrow deeper into the dermis . The tick then begins feeding, sucking the host’s blood up through a channel located between the structures.
Here is an animation of the attachment process :
But if ticks suck blood out of their hosts, how do they transmit infection into them? Linden Hu, M.D., Professor of Medicine at Tufts University explains. “The organism that causes Lyme disease, Borrelia burgdorferi, lies dormant . The organism becomes active only after exposure to the warm blood meal entering the tick’s gut. Once active, the organism enters the tick’s salivary glands. As the tick feeds, it must get rid of excess water through the salivary glands. Thus, the tick will literally salivate organisms into the wound, thereby passing the infection to the host” .
According to Dr. Hu, substances should not be applied to an embedded tick in attempts to make it loosen its grip. He warns “do not use a smoldering match or cigarette, nail polish, petroleum jelly (e.g. Vaseline), liquid soap, or kerosene because they may irritate the tick and cause it to behave like a syringe, injecting (its) bodily fluids into the wound” . A popular video circulating on the Internet demonstrates the application of a drop of Peppermint essential oil onto an embedded tick, which subsequently “backs out” of its attachment on the skin and starts to crawl away. Unfortunately, as Dr. Hu describes, it’s likely that the irritant action of Peppermint essential oil may have caused disease causing organisms to be injected into the wound before the tick withdrew. Incidentally, Peppermint was the least effective of eight essential oils tested for tick repellency, and vetiver was twice as potent (38).
What should I do if I get bitten by a tick?
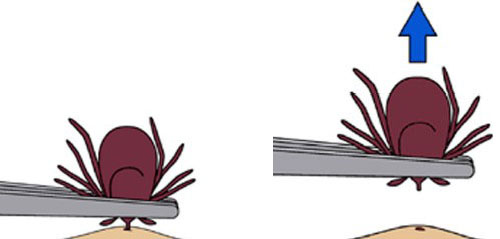
First, don’t panic. The U.S. Centers for Disease Control (CDC) advises taking the time to properly remove a tick to help reduce the chances of an infection. Applying a noxious substance to the tick is not recommended. Grasp it with fine-tipped tweezers as close to the skin as possible (grasping the tick’s body with tweezers may squeeze its abdominal contents into the wound or can cause the body to break off, leaving mouth parts embedded).
Pull SLOWLY and steadily straight upwards (see illustration). Avoid jerking movements or twisting the tick as they can cause the tick’s body to break off, leaving mouth parts embedded in the skin.
A variety of tick-removal tools are available, but those that work by pulling straight upward/out are preferred. There is a popular tool newer on the market that “twists” the tick round and round while removing it. This sort of tool is not recommended as twisting movements may stimulate the tick to salivate into the wound, possibly injecting infectious organisms. And, tick barbs are straight, not spiral.
If the body of the tick comes out but head/mouth parts remain in the wound, don’t worry. Try grasping the remaining parts with tweezers and gently pull to remove them. If that doesn’t work, wash the area carefully with soap and water or an alcohol-based hand sanitizer. It’s acceptable to dab a little antibiotic ointment on the area and cover it with a band aid; alternatively the CDC says you can just leave the area alone. There is no evidence proving that mouth parts alone can transmit disease once the tick’s body is removed .
I pulled it out. Now what?
Place the tick in a plastic baggie or jar with a lid. Don’t squeeze or crush the tick. Wash the bite area, your hands, and the tweezers/tick removal tool in warm, soapy water. If you’re out hiking in the woods, rinse the area, and the tools, with bottled water or use an alcohol-based hand sanitizer.
Should I bring the tick to be tested?
This is a matter of debate. Science blogger Meghan Rosen describes two points of view about tick testing. In 2015 Rosen interviewed Dr. Sunil Sood, pediatric infectious disease specialist at Hofstra North Shore-LIJ School of Medicine, who stated “testing for bacteria is a waste of time and money” . Rosen summarizes Dr. Sood’s reasoning.
First, the presence of host blood in the tick’s gut may interfere with test results. Second, even if a tick tests positive for bacteria it doesn’t necessarily mean an infection was transmitted into the host’s body. Finally, a tick which tests negative doesn’t rule out disease.
Since ticks are tiny and their bites virtually painless and because they like to hide in hidden body creases and folds, a person may be unaware of having being bitten by another tick which *was* infected. Therefore, a tick which tests negative for infection may impart a false sense of security to the person who brought the tick for testing .
Finally, laboratory testing destroys the tick and eliminates the possibility of doctors making an identification which can help guide treatment choices. Dr. Sood says: “I don’t want to be looking for Lyme disease when it was a lone star tick” .
However, microbiologist Stephen Rich of the University of Massachusetts Laboratory of Medical Zoology opines that the intent of tick testing is not to diagnose disease in humans but is of significant benefit in epidemiological disease surveillance .
If possible, take the tick you removed and placed in a baggie or jar with you when visiting a medical provider so the clinician can identify which kind of tick it is and initiate the proper treatment pathway.
Should I get Tested?
Depending on the geographic area where the bite occurred (e.g. a Lyme endemic area vs. an area where the illness isn’t common) you may choose to contact a medical provider or adopt a “wait and see” approach. In the meantime it’s imperative to monitor for symptoms such as:
- Rash – a “bulls-eye” rash called erythema migrans, occurring in many but not all cases of Lyme Disease. The rash can occur at the site of the bite or anywhere else on the body (see photo) and generally appears 3-30 days after an exposure.
- Fever
- “Crushing” joint aches or pains
- Extreme fatigue
- Severe headache
You may choose to see a medical provider right away if you live in an area where Lyme Disease is endemic. Physicians can evaluate each individual situation and decide if treatment benefits outweigh possible risks. Pregnant women who have been bitten by a tick should always see their care provider as soon as possible .
What tests are there for Lyme Disease?
The presence of an erythema migrans (“bulls-eye”) rash is considered an absolute diagnostic criterion for Lyme disease and no further confirmatory testing is necessary . The medical provider will begin treatment immediately.
The enzyme-linked immunosorbent assay (ELISA/EIA) and the Western Blot are “indirect” serological tests that look for a bodily response to an infectious agent (where the body forms antibodies) rather than looking for the actual presence of an infectious agent. However, since it may take 2-4 weeks after a tick bite to produce antibodies to Lyme bacteria, a low level may lead to negative test results. If the ELISA test is positive for Lyme antibodies, a more in-depth Western Blot test is performed. This test looks for the presence of certain “bands” on an immunoblot “paper” .
The polymerase chain reaction (PCR) test looks for the presence of Lyme bacteria DNA sequences in blood. The presence of Lyme DNA sequencing in the blood sample is considered diagnostically positive. However, a negative result does not confirm the absence of infection .
No Lyme test from any laboratory in the world can guarantee 100% reliable results. This is why medical providers elicit a careful history from the patient and perform a thorough clinical exam in conjunction with lab results. This yields the most complete “picture” of the patient’s condition .
Good news and bad news
The good news: a majority of people infected with Lyme Disease respond quickly to treatment with antibiotics. The earlier a treatment protocol is initiated, the better the chances of a cure . The bad news: smaller subgroups of people may not respond to antibiotic treatment and their symptoms can linger for extended periods. Termed “Post-Treatment Lyme Disease Syndrome” (formerly known as “Chronic Lyme Disease”), this condition can be frustrating and life-altering for sufferers . In these cases, finding a practitioner with Lyme-specific expertise (an infection control specialist or “Lyme Literate” doctor) is important in helping people reclaim quality of life.
Prevention
All medical professionals agree that preventing tick bites in the first place is key. Choosing light colored clothing before outdoor excursions makes it easier to spot any “hitchhiking” ticks. It’s also advised to wear long sleeved shirts and pants and to tuck pants cuffs into socks so bare skin isn’t exposed. However, being dressed in this manner makes it easy to overheat in hot weather. An alternative is to wear socks, shoes, clothing, and a hat treated with permethrin (a synthetic compound derived from chrysanthemum flowers) which allows for greater comfort, while conferring superior protection against ticks .
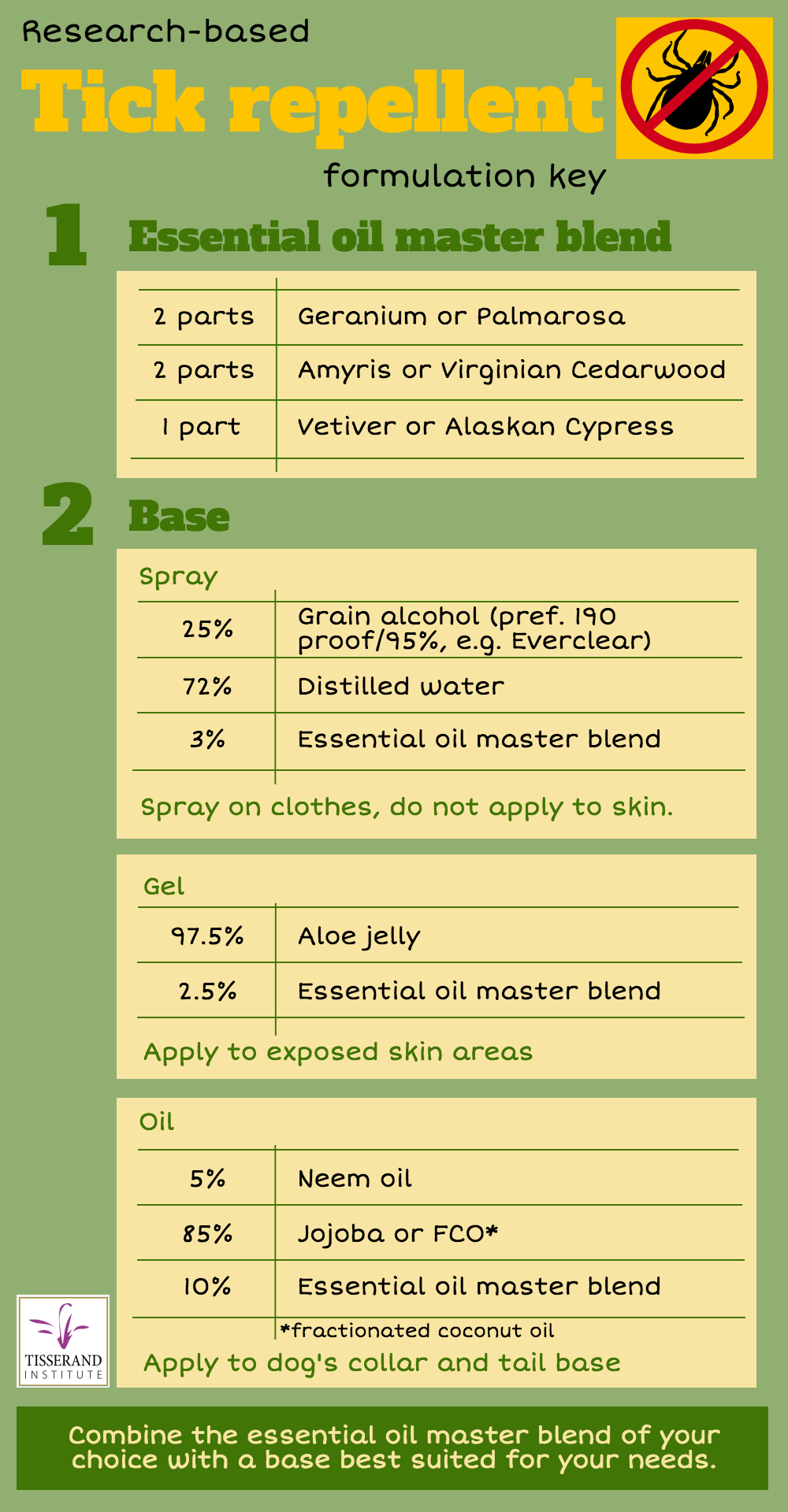
There is promising research exploring the use of essential oil and herbal preparations as tick repellents. In some cases, these formulas rival DEET, permethrin, picaridin, or IR3535, all CDC-recommended tick repellents . An effective tick repellent will have both high volatile ingredients for immediate impact, and low-volatile ingredients, for long-lasting efficacy. One tried and tested high volatile essential oil is Geranium, and we know that both the oil and its major constituents, geraniol and citronellol, repel ticks (28,29,30,31). Palmarosa (Cymbopogon martini), which is high in geraniol, oil is likely to be equally effective.
Two viable options for medium volatility tick repellents are Amyris (Amyris balsamifera) and Virginian Cedarwood (Juniperus virginiana) (32,33). For low volatility, Alaskan Cypress (Chamaecyparis nootkatensis) would be an ideal choice, as its constituents have been extensively tested for tick repellency (34,35,36). However, an alternative and easier-to-find essential oil would be Vetiver (Chrysopopon zizanoides, syn: Vetiveria zizanoides) (37,38). See infographic for a formulation based on this research.
Start with making the master blend. Choose one from each row of essential oils eg. Palmarosa, Amyris and Alaskan Cypress. Then depending on how you want to use the repellent, chose one of the three bases to mix the complete blend in. Spray is most suitable for application to shoes, clothing, backpacks etc., and is safe even for children over the age of 2. We have seen many formulations online containing vodka, witch hazel distillate, cider vinegar or hydrosols. Note that none of these will effectively solubilize essential oils! Also, the water must be distilled, and the formulation should be used within a few weeks. If not wearing long pants and long sleeves – or if you want to avoid alcohol – use the gel and apply to exposed skin areas. Please note that “aloe jelly” is not the same thing as “aloe gel”. Aloe gel is 99% water, and will not solubilize essential oils. Aloe jelly also contains added thickeners, and you can easily mix in essential oils. For dogs, use a drop or two of the oil formulation on the collar and tail base. Please do not use for cats. There’s no reason why you couldn’t use just the essential oils for shoes, pant legs, hats etc.
Being outdoors confers many benefits to one’s health: beauty, relaxation, and an appreciation for all that nature offers. Don’t let a fear of ticks ruin your alfresco experiences!
 References
References
1.”Tickborne Diseases of the United States”. Centers for Disease Control website. https://www.cdc.gov/ticks/diseases, retrieved May 18, 2017.
2. “Ticks”. Purdue University Medical Entomology website. https://extension.entm.purdue.edu/publichealth/insects/tick.html, retrieved May 19, 2017.
3. “Black Legged Ticks”. University of Rhode Island Tick Encounter Center. www.tickencounter.org/tick_identification/deer_tick, retrieved May 23, 2017.
4. “About Ticks and Lyme Disease”. Lyme Disease.org website. https://www.lymedisease.org/lyme-basics/ticks/about-ticks, retrieved May 19, 2017
5. “Tick Borne Diseases-EMedicine Medscape. Medscape.com website. http://emedicine.medscape.com/article/786652-overview, retrieved May 20, 2017.
6. “What are Ticks?” Identify US website. https://identify.us.com/idmybug/ticks/tick-FAQS/what-are-ticks.html, retrieved May 20, 2017.
7. “CDC – Babesiosis – Resources for Health Professionals”. Centers for Disease Control website. https://www.cdc.gov/parasites/babesiosis/health_professionals/index.html#tx, retrieved May 15, 2017.
8. ”A Brief History of Lyme Disease in Connecticut.” Connecticut Department of Public Health website. http://www.ct.gov/dph/cwp/view.asp?a=3136&q=3885062, retrieved May 5, 2015.
9. “Lyme in 80+ Countries Worldwide”. Lyme Disease Association website. http://www.lymediseaseassociation.org/index.php/about-lyme/cases-stats-maps-a-graphs/940-lyme-in-more-than-80-countries-worldwide, retrieved May 5, 2017
10. Riffenburgh, B. Encyclopedia of the Antarctic (v. 1) 1st Edition. Routledge Publishers, Abingdon-on-Thames, 2006, pg 335.
11. “2015 – Google Searches on Lyme Disease Jump to their Highest Level”. http://danielcameronmd.com/2015-google-searches-on-lyme-disease-jump-to-their-highest-level/, retrieved May 16, 2017.
12. “Mother posts scary warning to parents about tick paralysis after young daughter can’t walk”. New Hampshire 1 news website, www.nh1.com/now, retrieved May 20, 2017.
13. Richter D, Matuschka FR et al. “How ticks get under your skin: insertion mechanics of the feeding apparatus of Ixodes ricinus ticks”. Proceedings of the Royal Society B website. http://rspb.royalsocietypublishing.org/content/280/1773/20131758, retrieved May 13, 2017.
14.”Watch a Tick Burrowing Into Skin in Microscopic Detail”. Smithsonian magazine website. http://www.smithsonianmag.com/science-nature/watch-a-tick-burrowing-into-skin-in-microscopic-detail-6649718/
15. “What to do After a Tick Bite to Prevent Lyme Disease.” Up-To-Date website. https://www.uptodate.com/contents/what-to-do-after-a-tick-bite-to-prevent-lyme-disease-beyond-the-basics#H2), retrieved May 20, 2017.
16. “Tick Removal”. Centers for Disease Control website. http://www.cdc.gov/lyme/removal/index.html, retrieved May 5, 2017.
17. “Lyme Transmission”. Centers for Disease Control website. http://www.cdc.gov/lyme/transmission.index.html, retrieved May 7, 2017.
18. “Lyme Treatment”. Centers for Disease Control website. http://www.cdc.gov/lyme/treatment/index.html, retrieved May 13, 2017.
19. “Lyme Signs and Symptoms”. Centers for Disease Control website http://www.cdc.gov/lyme/signs_symptoms/index.html, retrieved May 15, 2017.
20. Rosen, M. “Five reasons to not totally panic about ticks and Lyme disease”. Science News website, https://www.sciencenews.org/blog/growth-curve/five-reasons-not-totally-panic-about-ticks-and-lyme-disease, retrieved May 17, 2017.
21. “Lyme Disease Workup”. Medscape website, emedicine.medscape.com/article/330178-workup, retrieved May 17, 2017.
22. Brenner, C. “Understanding the Western Blot”. Lyme Disease.org website, https://www.lymedisease.org/wp-content/uploads/2014/08/Image13-link-pdf-brenner.pdf, retrieved May 22, 2017.
23. “Diagnosis and Testing”. Centers for Disease Control website. https://www.cdc.gov/lyme/diagnosistesting/index.html, retrieved May 22, 2017.
24. “Treatment”. Centers for Disease Control website. https://www.cdc.gov/lyme/treatment/index.html, retrieved May 22, 2017.
25. “Post-Treatment Lyme Disease Syndrome.” Centers for Disease Control website. https://www.cdc.gov/lyme/postlds/index.html, retrieved May 23, 2017.
26. “Permethrin Facts”. United States Environmental Protection Agency. www.epa.gov/oppsrrd1/REDs/factsheets/permethrin_fs.htm, retrieved May 5, 2017.
27. “Preventing Tick Bites”. Centers for Disease Control website. https://www.cdc.gov/ticks/avoid/on_people.html, retrieved May 24, 2017
28. Bissinger, B. W., Kennedy, M. K., & Carroll, S. P. (2016). Sustained efficacy of the novel topical repellent TT-4302 against mosquitoes and ticks. Medical and Veterinary Entomology, 30(1), 107–111. http://doi.org/10.1111/mve.1215
29. Bissinger, B. W., Schmidt, J. P., Owens, J. J. et al (2014). Activity of the plant-based repellent, TT-4302 against the ticks Amblyomma americanum, Dermacentor variabilis, Ixodes scapularis and Rhipicephalus sanguineus (Acari: Ixodidae). Experimental and Applied Acarology, 62(1), 105–113. http://doi.org/10.1007/s10493-013-9719-1
30. Ferreira, L. L., Oliveira Filho, J. G. de, Mascarin, G. M. et al (2017). In vitro repellency of DEET and β-citronellol against the ticks Rhipicephalus sanguineus sensu lato and Amblyomma sculptum. Veterinary Parasitology, 239(March), 42–45. http://doi.org/10.1016/j.vetpar.2017.04.021
31. Tabanca, N., Wang, M., Avonto, C. et al (2013). Bioactivity-guided investigation of geranium essential oils as natural tick repellents. Journal of Agricultural and Food Chemistry, 61(17), 4101–4107. http://doi.org/10.1021/jf400246a
32. Carroll, J. F., Demirci, B., Kramer, M. et al (2017). Repellency of the Origanum onites L. essential oil and constituents to the lone star tick and yellow fever mosquito. Natural Product Research, 6419(February), 1–6. http://doi.org/10.1080/14786419.2017.1280485
33. Eller, F. J., Meer, R. K., Behle, R. W. et al (2014). Bioactivity of cedarwood oil and cedrol against arthropod pests. Environmental Entomology, 43(3), 762–766. http://doi.org/10.1603/EN13270
34. Dietrich, G., Dolan, M. C., Peralta-Cruz, J. et al (2006). Repellent activity of fractioned compounds from Chamaecyparis nootkatensis essential oil against nymphal Ixodes scapularis (Acari: Ixodidae). Journal of Medical Entomology, 43(5), 957–961. http://doi.org/10.1603/0022-2585(2006)43[957:RAOFCF]2.0.CO;2
35. Jordan, R. a, Dolan, M. C., Piesman, J., & Schulze, T. L. (2011). Suppression of host-seeking Ixodes scapularis and Amblyomma americanum (Acari: Ixodidae) nymphs after dual applications of plant-derived acaricides in New Jersey. Journal of Economic Entomology, 104(2), 659–664. http://doi.org/10.1603/EC10340
36. Panella, N. A, Dolan, M. C., Karchesy, J. J. et al (2005). Use of novel compounds for pest control: insecticidal and acaricidal activity of essential oil components from heartwood of Alaska yellow cedar. Journal of Medical Entomology, 42(3), 352–358. http://doi.org/10.1603/0022-2585(2005)042[0352:UONCFP]2.0.CO;2
37. Campos, R. N. de, Nascimento Lima, C. B., Passos Oliveira, A. et al (2015). Acaricidal properties of vetiver essential oil from Chrysopogon zizanioides (Poaceae) against the tick species Amblyomma cajennense and Rhipicephalus (Boophilus) microplus (Acari: Ixodidae). Veterinary Parasitology, 212(3–4), 324–330. http://doi.org/10.1016/j.vetpar.2015.08.022
38. Meng, H., Li, A. Y., Costa Junior, L. M. et al (2016). Evaluation of DEET and eight essential oils for repellency against nymphs of the lone star tick, Amblyomma americanum (Acari: Ixodidae). Experimental and Applied Acarology, 68(2), 241–249. http://doi.org/10.1007/s10493-015-9994-0




Thank you so much for this very informative article. I really appreciated the science and also the graphics included. Here’s to a tick-free summer!
We have used the twisting tick sticks successfully on our dogs. When our vet pulled out a tick straight with the tool they use, the head was left in and they just left it. It left a bump that finally went away after a month or so. So now I am confused on which tick sticks to use since we had good luck with the twisting ones.
Thanks,Ann, for posting!
Thank you for this article
Question, what does 2 parts and 1 part equate to?
I.e. how many drops are in 2 parts? And how many drops are in part? Is it depend on the quantity of the base used? Thank you
Renee
The “parts” refers to your choice of measurement ie. grams, ounces, ml., tsp. Etc. When measuring in parts you are keeping the proportions the same. For the master recipe you could do 2ml of geranium, 2ml cedarwood, 1ml vetiver; this would fit nicely in a 5ml dropper bottle for future use (keep refrigerated).